Readings in Humanistic Psychiatry: New Models of Psychiatrist- Patient Relationships
New Models of Psychiatrist- Patient Relationships
The psychiatric profession is at an unusual stage of its development. We know far more about the workings of the brain today than ever before. There is now a uniform diagnostic system with clear criteria for each disorder. We have a wide variety of new psychotropic medications that are generally better tolerated than those available just a decade ago. By all accounts this should be a good time to be a psychiatrist (if there ever is a good time).
Despite our many advances, there's still a lot of grumbling going on about psychiatrists.
It's very common to hear patients, family members, and mental health professionals bemoan the quality of current psychiatric care in America. Even people who work with, like, and respect psychiatrists have some legitimate complaints. And at the other end of the spectrum there are people who would like to see the entire psychiatric profession abolished altogether. So how can we understand this discrepancy between our view of ourselves as a profession that is making rapid advances in helping people and our sagging reputation among the general public?
Anyone who comes into contact with our mental health system, either for treatment themselves or for the care of loved ones, immediately becomes aware that we shrinks occupy a unique and powerful position. Decisions about medications, housing, eligibility for benefits, referrals for other treatments, and even decisions about whether involuntary treatment should take place are typically handled by the psychiatrist.

Of course this is ironic. The psychiatrist is usually the person who has the least amount of actual contact with the patient of all the professionals that may be involved in the person's care. Five to fifteen minute appointments every three to six months are now the industry standard for seeing patients in the public sector. It often takes several months just to get an appointment. A busy psychiatrist may see in the neighborhood of thirty patients per day. Sometimes we can barely remember who the patient is, let alone details of their histories, without consulting their chart. Yet the mental health system treats us as though these were still the days when we saw patients for an hour at a time, several days per week and were intimately familiar with their lives.
Believe it or not, not every psychiatrist believes that medications are the solution to every human problem. But our role in mental health systems has gradually evolved to a point where psychiatrists are used primarily as dispensers of medications. And bad things can happen when we don't do a good job of prescribing these powerful medications. Of course the obvious concern is that the patient might not get better if the medications aren't chosen and dosed properly but that's only a small part of the problem.
When we shrinks goof up with medications we can cause problems that look an awful lot like the symptoms that we were trying to treat in the first place. Giving the wrong medication - or more commonly - combinations of medications, can lead to agitation, confusion, irritability, social withdrawal, depression, mania, and even psychotic symptoms.
A vicious cycle can result, with the psychiatrist believing the person's illness has gotten worse and prescribing more medications in an attempt to reduce the symptoms caused by the original drugs. Many patients end up taking so many medications that it is essentially impossible to tell whether each one is helpful or is causing more problems than the patient started with.
Relationships with Psychiatrists
On the surface it would seem that having a good relationship with a psychiatrist should be an easy thing to accomplish. After all, we're trained to understand people. We know about how people communicate and the types of relationships that they have. Any psychiatrist should be able to present him or herself as a sympathetic person. The vast majority of psychiatrists genuinely want to help people. But a lot of obstacles to forming a good working relationship with a psychiatrist can crop up. Some of these obstacles are more obvious than others.
Attitudes, expectations, and misconceptions can all lead to problems. Consider the popular image of psychiatrists. We're generally imagined to speak with an Austrian accent and have our patients lie on funny couches. People have come to expect that we'll be good listeners. Some arrive with the hope that we'll help them to understand themselves in new and helpful ways. They may anticipate that we will be quite concerned with unconscious material and be able to provide insights into the reasons that they think and feel the way they do. Many are unprepared for the sorts of cursory symptom checklists that have come to characterize psychiatric visits these days. A lot of people leave our offices disappointed and disillusioned.
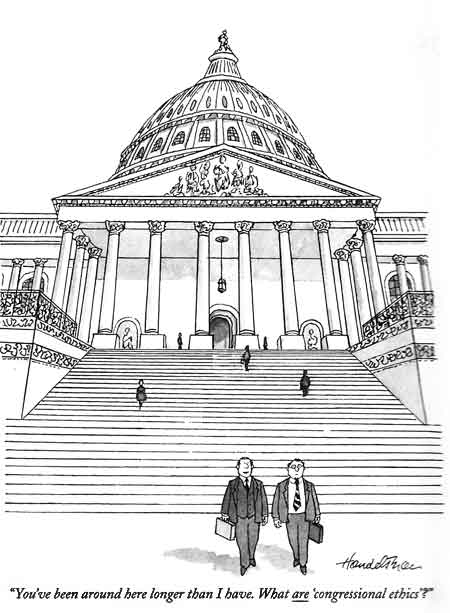
Some people believe that we're some type of mad scientists. They fear that we'll be able to change them in powerful ways, even thinking that we can change the contents of their minds without their awareness or participation. Others see us as inept bunglers who are often far shorter in common sense than the people that we're trying to treat. A few crackpots even believe that our profession is inherently evil.
Rarely do people see psychiatrists in the way that we like to see ourselves. Many psychiatrists believe themselves to be hard core scientists, struggling to correct chemical imbalances that cause mental illnesses - imbalances that only they can really understand. Psychiatrists coming out of training programs today have been trained to think within a medical model. We may wear white coats to remind everyone that we're really doctors, even though most of us don't do well with the bodily fluids that the white coats are intended to protect us from.
There are a lot of names for the kind of thinking found within that medical model. Linear thinking, rational thinking, left brain thinking. Perhaps the best is reductionistic thinking.
The term implies that if one could break down the component parts of the brain and understand each of the parts adequately, one could truly understand the human mind and predict how it would respond in any given situation. There is nothing wrong with this sort of thinking. It's the same kind of thinking that good automotive mechanics use when fixing cars. It's responsible for advances in medications and in our understanding of the brain. In fact the selection process for this type of thinker begins early in our school years and continues throughout premedical programs in college. It is essentially impossible to get into medical school and become a doctor if you aren't pretty good at reductionistic thinking.
As a group we psychiatrists tend to be a little defensive about our credentials as scientists and may try extra hard to portray ourselves in a "scientific" light. Most of us were not at the top of our medical school classes. People are always getting us mixed up with psychologists. We've all been asked "are you a real doctor?" on far too many occasions. Some of our families were quite disappointed that we didn't choose more glamorous and "medical" specialties. Many patients seeing psychiatrists for the first time are surprised to learn how different we are from what they had come to expect.
Patients commonly want to feel understood and accepted. Like most of us, they would also like to be admired, or at least to have their concerns validated. They often want to feel better right away. The psychiatrist may be, at least unconsciously, expected to know what is wrong and to make things better without having to ask a lot of questions to accomplish this. Patients often resent being asked for information, especially when the questions are difficult for them to answer. When a medication is prescribed they, understandably, expect that it will produce the desired results immediately, or at least within a day or two.
While those desires are understandable, that's not quite how things work in modern psychiatry. Many people are disappointed to learn that they'll need to stay on a new medicine for a couple months before they'll be able to tell if it works. And even when the medicines are effective it's rare for anyone to rave about the way they feel on them. Many times patients need to count on other people to tell them if the drugs are really making a difference because the answer isn't so obvious to the individual who's taking them.
Psychiatrists are trained to approach human problems in a particular way. We want to know things like "When did the problem begin?" What was going on when the problem started? Has it been present continuously or does it come and go? What makes it better? What makes it worse? Does anyone in the family have a similar problem? And so on. A good psychiatric diagnosis is always based on the course of symptoms as they occur throughout the patient's life.
We're also particularly prone to asking people to compare how they think and feel now with how they were at some point in the past. It's very hard to evaluate the effects of medications without such comparisons. Yet most of us can't really recall how we thought or felt a month ago compared with today. This is a hard task for anyone's memory apparatus to accomplish and many of our patients have more difficulty with this sort of recall than the average person.
So a clash of goals and expectations seems inevitable as psychiatry becomes an increasingly "medical" discipline. And certain realities of the current mental health system only make matters worse. It's very difficult to talk with someone, form a good working relationship with them, define their problem, discuss options and strategies for dealing with the problem, get input from family or other professionals, prescribe a medication, discuss the expected benefits and the amount of time it will take for them to develop, and review side effects and potential drug interactions - all in the course of fifteen minutes or less. Yet psychiatrists have to try to do this all the time.
We're always in the position of having too little time to accomplish what we want to do for people. We always have to make decisions with too little information to go on. It's not surprising that we psychiatrists would be a little anxious or defensive about all of this. And many of us came into the field because we were a bit more anxious or neurotic than our classmates to begin with. The combination of anxiety and power can do strange things to people.
Complaints that patients have about their psychiatrists
It's easy to predict some of the complaints that patients have about their psychiatrists. Some common ones - and this is a very partial list - include:
- My psychiatrist doesn't spend enough time with me.
- He doesn't really listen to me or try to understand me as a person.
- He doesn't explain things to me.
- She sees me as just a collection of symptoms.
- I am only understood in terms of my diagnosis.
- I have to wait too long in the waiting room.
- If I really have a problem I can't get in to see my doctor.
- My doctor uses language that I can't understand.
- He prescribes medications regardless of the problems that I come in with.
- He doesn't include me in decisions about my own life.
- She forgets how much these medications cost.
- My doctor doesn't return my phone calls.
- I am taking so many medications that I can't tell if they're helping or not.
- My doctor disregards my spiritual beliefs.
- My doctor treats me as though I were less than equal.
- The psychiatrist calls me by my first name but wants me to call him Doctor.
- He is never interested in my own ideas about my problems.
- Every time that I see a new psychiatrist I get a new diagnosis.
Complaints that psychiatrists have about patients
It may come as a surprise to learn that some psychiatrists are not entirely happy with the current state of affairs either, especially those that were primarily trained as psychotherapists. Some common complaints that psychiatrists may reveal - in selected company - include:
- People just want to chat instead of talking about the important things that need to be covered.
- We are expected to understand complex problems and come up with solutions but aren't provided with enough information to do the job.
- Patients ask for advice but rarely follow it.
- Patients always save the most important topics for the end of the meeting, then get upset when we don't have time to discuss them.
- People expect miracles.
- Patients rarely take their medications the way that we prescribe them.
- We are often blamed - or even sued - when things go wrong but we rarely get credit when things go well.
- We are held too responsible for things that we cannot control, especially the way patients behave.
- People are always equating the bad things that our patients may do with our own talents as psychiatrists.
- Patients expect us to be available whenever they want us.
- Family members sometimes expect to be given as much time as the patients themselves.
- There is often no place to send patients back to live after they have been in the hospital.
How to make the best use of your time with a psychiatrist
When people need to see psychiatrists it makes sense to make the visit as productive and helpful as possible. Taking steps to actively influence one's treatment can also affect the power balance within the relationship. The idea that patients should somehow be less than equal partners in a relationship designed to affect the quality of their own lives is pretty silly when you think about it.
Some simple things that consumers of psychiatric services can do to improve their care include:
- Before you see a psychiatrist give some thought to defining the problem that you want help with.
- Don't expect the doctor to magically understand your problem. You'll probably be disappointed in the care that you receive if you do.
- If you're starting with a new psychiatrist try to have records available from prior treatments. If possible have them sent to the psychiatrist's office in advance.
- Bring a list of current medications and dosages. Include non psychiatric medicines, over the counter drugs, and herbal supplements.
- Be as honest as possible about your medication compliance. Being dishonest about how often you're not actually taking the medications can easily lead the doctor to conclude that you need more medicine than he is already prescribing. A good doctor-patient relationship should be built upon openness and honesty, from both sides.
- Learn as much as possible about the disorder that you (or your loved ones) suffer from. Information about the various mental disorders and medications used to treat them is widely available on the Internet now. It makes good sense to become as much of an expert on your own condition as possible.
A few useful mental health websites
Medscape/WebMD
- Medline access, free CME's, Lots of archived articles, frequent updates.
Medscape/Drug Interaction
- A very good drug interaction checker. Anytime two or more medications are prescribed it's a good idea to check for interactions between them.
Crazy Meds
-Lots of medication facts, especially from a consumer perspective.
MentalHealth.com
-Wonderful source of info on medications and disorders, includes a computerized diagnostic program.
Texas Department of State Health Services
-Summary of best practice decision trees for treating major mental illnesses with medications
- Whenever you take a psychiatric medication know what it is supposed to do. Define the target symptoms that it is supposed to affect. Try to keep track of whether these target symptoms are getting better or worse. Using a symptom rating sheet or even just a calendar to track changes can be helpful.
- If it is hard for you to tell if your symptoms are getting better (and this is pretty common) enlist the assistance of people that you trust. Have them make observations about your progress as they see it. Provide that information to the psychiatrist. The better information that he has, the easier it will be for him to make good treatment decisions.
- Use advance psychiatric directives to make your wishes about treatment clearly stated in case you are ever hospitalized and felt to be incompetent to make decisions about your own care. Make sure that your psychiatrist has a copy.
- Try to be up front about what you really want from a psychiatrist. If you're a family member or a mental health professional and are trying to have someone's problematic behaviors brought under control be open and direct about that.
- Be willing to spend at least as much time and energy shopping for a psychiatrist as you would when looking for a used automobile.
- Realize that recovery from severe mental illnesses is usually a lengthy process and will look different for everyone.
- When problems or disagreements with psychiatrists arise realize that is rarely helpful to confront his view of himself an expert. Statements like "my cousin is a nurse and she says you should do such and such" or "according to what I have read about this..." will often be rejected by the psychiatrist immediately. Keep in mind the size of an ego that a person needs to have to be a psychiatrist and avoid direct challenges to it.
- Understand that we shrinks are as sensitive to evaluation, praise, and criticism as anyone else. If you like something that your psychiatrist did, or if he upset you in some way, sending a note to him or his boss can go a long way to shaping future behavior.
- If possible, attach numbers to symptoms that are being treated. e.g. "Johnny's sleep increased from 3 hours per night to 6 hours per night over the past month." Or " my voices decreased in frequency by about 60% when we switched to the new medication ". We psychiatrists often have a tendency to think that everything should have a number attached to it. It's more "scientific" that way.
- Realize that even if you do all of these things it will still be important to have a good relationship with the psychiatrist's nurse. The nurse is usually the person that controls access to the psychiatrist's time and attention and can do a lot to shape the way that he will respond to a given situation.
Twenty Questions That You May Want To Ask Your Psychiatrist
Patients will often say that they don't know what questions they should be asking their psychiatrist. Or they have questions but forget to ask them. Or that there just isn't enough time for questions. Sometimes they don't want to risk offending the psychiatrist by asking questions that may be viewed as "stupid". The following is a list of twenty questions that anyone would be justified in asking about their diagnosis and treatment. Asking all twenty in the same session may be met with some resentment and would take a lot of the available time. But it is a good idea for anyone to get answers to these important questions as their relationship with the doctor goes on.
Diagnosis Questions
- 1) What is my diagnosis?
- 2) What symptoms or problems led you to make this diagnosis?
- 3) Is there a chance that I might actually have a different disorder?
- 4) Would the different diagnosis change my treatment in any way?
- 5) Is there any other information that is needed to arrive at a clear diagnosis?
Treatment Questions
- 6) What medications are commonly used to treat my condition?
- 7) What is the medication supposed to do?
- 8) How long does the medicine usually take to work?
- 9) What signs of improvement might I notice first?
- 10) Will I continue to notice new benefits if I keep taking the medicine?
- 11) Are there signs of improvement that I might not notice? If so, what should I ask my family and friends to watch for?
- 12) What alternatives are there to this medicine?
- 13) Are there non-medication options that might be helpful? (i.e. exercise, herbs, talk therapies, etc.)
- 14) Has the combination of medications that I am taking ever been researched?
- 15) If my combination of medications is "experimental" have the customary treatments been tried first?
- 16) What side effects might I experience with this medicine?
- 17) Will the side effects disappear over time? Might they get worse?
- 18) What should I do if I experience side effects?
- 19) How might this medication interact with other medicines (or drugs/alcohol) that I am taking?
- 20) Do you have any suggestions about where I can learn more about my condition and its treatment?
One can easily imagine that the contents of this chapter will not be warmly embraced by all psychiatrists. We're usually pressed for time. We don't always enjoy having our decisions questioned. Some of us are pretty sensitive and even a tad grandiose. Questioning the idea that every human problem should be met with a medication may be resented.
The inequalities present in many patient-psychiatrist relationships have been present for a long time and there is little incentive on our side to make changes. There are all sorts of reasons why just doing what we've always been doing will seem like the only sensible option.
Yet most of us would have to admit that we'd want our loved ones to receive better treatment than most psychiatric patients currently get. We would want the doctor to spend an adequate amount of time with our family members and to take a real interest in their care. We'd want more for them than a few quick questions followed by yet another prescription for an expensive new medicine. We'd want our loved ones to be treated as respected equals rather than as a diagnostic condition.
Ironically, while psychiatrists are always quick to trumpet our new scientific breakthroughs into the mysteries of the mind, the real progress lying ahead is likely to involve new models of doctor-patient relationships and better living environments for our patients rather than innovations in medication.
Different models for psychiatrist-patient relationships
Most psychiatrists have been so immersed in a "medical model" of treatment relationships from the very beginning of our training that it is hard for us to step back to take an objective look at the way that we deal with people. We are the experts. The patient is the one with the problem. We diagnose the problem and prescribe a treatment. The patient's job is to comply with the prescribed treatment. If they don't comply, and problems result, then it is clearly their own responsibility.
Pretty simple really. It's just that a great many mentally ill people don't see things in quite this way. The medical model doesn't work very well for a lot of these people.
Many people with mental illnesses can't tell that they are ill in the first place. They may not be able to notice or recognize any benefits from the treatments that we prescribe. A lot of them end up in our offices against their will - someone else has insisted that they come and dragged them in over their bitter protests.
Clients can arrive with very different agendas than "receiving treatment". They may want housing or support services, or they need to have forms filled out to receive entitlements. They can be a little ambivalent about buying into a relationship model in which they're told what they should do and their role is just to follow directions. Especially if they barely know the doctor as a person and have no real reason to believe that the doctor would have their best interests at heart.
Patients usually learn that direct opposition to the established model will only bring them trouble. They may be viewed as more symptomatic and have their medications increased. The psychiatrist may refuse to see them and they'll end up having to wait a long time to see someone else. Families or case managers may pressure them to be more compliant. Hospitalizations can even result. So more covert ways to regain control in the relationship with the doctor are utilized.
Non-compliance rates with our prescribed medications typically are found to run at over 50 % in outpatient populations. Patients may play "medication Yahtzee" or take a medication that they like and disregard the rest. Sometimes they trade medications with other mentally ill people. They often miss scheduled appointments with us. When they do come they may tailor their presentation, exaggerating some problems or denying others depending upon what they want from us.
Ultimately it's the patient who has the final say in whether our prescribed treatments will be embraced or rejected. The idea that we psychiatrists would convince ourselves that we are in charge of these relationships is actually pretty goofy. Engaging in power struggles that we can't possibly win is a position that we find ourselves in all of the time.
Directors or consultants ?
A more sensible type of relationship with our clients might be one in which we strive to achieve the role of trusted consultant to people that have significant problems in living. When you think about it the job of the modern psychiatrist is not that different from that of an optometrist.
People with severe mental illnesses have significant problems with the ways that their brains are structured and functioning. As a result, their complex pictures of reality - complete with emotions, motivations, and impulses to behave in particular ways - have gone awry. The distortions of reality may be of a different kind and degree than the simple visual problems that optometrists correct but the basic analogy holds.
When we prescribe a medication to someone it's similar to the optometrist putting lenses before a patients eyes. They ask "which looks better, number one or number two?". It is the patient who must decide which lens provides the picture of the world that looks best to him. And it's really the same for psychiatrists and our patients.
When we prescribe psychotropic medications we are essentially holding up a lens before the brain. But when we ask "is this better or worse?" it's harder to get clear answers. It often takes weeks to months - even years in some cases - before the full effects of our medications become apparent. The changes can involve subtleties of thinking, behaving, and feeling that the patient may not even recognize. Many events may have taken place in the weeks before the medications began to work and cause-effect relationships might be hard to determine. If we're to be serious about helping these people finding a way for them to assess whether they get better or worse in response to a given treatment only makes sense.
So the modern psychiatrist's job is not just to medicate. We must also educate. We need to help clients learn how to determine whether medications are truly helping them. We should be teaching them what benefits to look for and what time course to expect. Honest information about what might happen if the medications are stopped should be provided.
Other professionals and family members should be seen as valued sources of information. The side effects that can result from treatment should be outlined and planned for. All of these things are just part of any respectful and sensible treatment approach.
But most important is the relationship in which this attempt to find the best medication or treatment to fit their malfunctioning brains takes place. We can't disregard the very real possibility that medications may work differently for an individual depending on who's hand they're coming from. It's very hard to separate out the effects of the beliefs, hopes, emotions, and behaviors that arise in the treatment relationship when trying to determine why someone did or did not improve in response to the treatment itself.
If our patients are busy resisting our efforts to help them, whether directly or covertly, they won't be able to participate in what should be a cooperative attempt to truly assess the effects of treatment on their lives. Finding the simplest and most effective treatment becomes a crap shoot if doctor and patient aren't working on the problem together.
To achieve a role as equal and respectful as that of "trusted consultant" psychiatrists will have to offer more than just prescriptions for new pills. Suggestions about lifestyle changes, non-medication therapies and different ways of conceptualizing the clients' problems will have to become part of our treatments.
Ideally, we'll come to know these people over time. In the best of cases we'll even be a part of the environment that they live in. If someone is becoming upset because a relationship has gone bad or there have been unusual stresses at the place they live in we'll understand them at that level rather than just using a simple equation of "more symptoms equals more medication."
Establishing trusting, symmetrical relationships with people suffering from severe mental illnesses involves a great deal of art and very little science. They are prone to seeing us in distorted ways and to live out old conflicts around authority that have been repeated since their early childhoods. When we're less than honest and open with them we relive these old patterns. If we are controlling or dictatorial with our clients we can reliably assume that they'll use ways to resist us that they utilized when they were little.
One valuable contribution from psychoanalysis has been the powerful emphasis on establishing and maintaining a genuine therapeutic alliance with the patient. Any treatment prescribed in the absence of such an alliance will have a lesser chance of being successful.
Playing with our patients?
A famous British psychoanalyst named Donald Winnicott may have provided the best perspective on the true nature of our relationships with our patients. Winnicott was best known for his ideas about "transitional objects" in childhood. As he pointed out, the child's teddy bear or special blanket belongs to a special class of things. It's not alive like Mommy or sister but it is very different from other inanimate objects. It occupies a place in a "transitional zone" where it is experienced both "objectively" and "subjectively". The differences between objective and subjective can be a little hard to keep straight though.
Let's look at an example using adults:
Subjective view of psychiatric treatment: Our work as mental health professionals is very valuable and important. Human lives are precious things and each person should be treated with all of the respect and reverence that we hold for our loved ones. Anything that we can do to alleviate suffering or to help another human being to have a better life is worthwhile, and makes our own lives better and more meaningful. Ours is truly an awesome responsibility.
Pretty heavy stuff when you think about it. Here is another way of looking at the same thing.
Objective view of psychiatric treatment: In a cosmos at least 30 billion light years across a tiny planet circles a little star, which is just one of a gazillion other stars. Both the planet and the star are moving at amazing speeds. On this little planet live about a billion relatively hairless ape-like creatures that have learned to make tools and to communicate by forcing air through two tightly stretched cords of flesh in their throats. Sometimes two of these primates sit in a room together. Both will inhabit their world for just a miniscule amount of time and neither one really knows anything about the nature of the universe. But one of the creatures is regarded as something of an expert and the other comes to him for help with problems, problems that may mean nothing at all in the grand scheme of things. The expert ape dispenses small tablets, or sometimes knowledge and advise, to the other. For this he is rewarded with pieces of paper with numbers and drawings on them.
As distasteful as this viewpoint might be compared to the first one, it's hard to say that it's inaccurate.
When someone embraces either the subjective or objective position alone bad things can happen. If one only sees the world through subjective eyes our responsibility to our clients can feel quite heavy and burdensome. We burn out or try to escape from work that is this serious and important. It's no surprise that psychiatrists have such an elevated suicide rate.
If one sees the world only through objective eyes then nothing really matters at all except for gratifying our own needs of the moment. We become sociopaths or bad politicians.
The key is to be able to hold both viewpoints simultaneously, and to live somewhere in between them most of the time. Winnicott believed that activities that take place in that crucial "transitional zone" are called "playing".
Golf is an excellent example of how playing works. On the one hand, as has been pointed out by many non-golfers, the game is really just walking around hitting a ball with a stick until it goes into a hole. It means absolutely nothing unless we agree to pretend to ourselves that it's actually important. Yet if you happen to talk in the middle of someone's backswing they might hit you with their stick.
Our relationships with our patients work best when we can inhabit that transitional zone with them. When we can agree to deal with their problems of living as though they are crucially important, while knowing at the same time that perhaps none of this matters at all and it's really only the effort that counts for anything. The best therapeutic relationships usually have a playful quality to them. So do the best human lives.
We all need that interplay between the objective and subjective views of life. If someone really believes that nothing about the human condition is truly important but they decide to behave as though this life were the most important thing in the universe, then everything will usually work out OK. If we believe that human life is the most precious thing ever created but decide to lighten up a bit and behave as though it isn't that big a deal we'll come out just fine too. It's always the extremes that get us, especially when we become certain that they're the only place where truth lies.
Playing is something that adults typically look down upon as an activity that befits only children. But is it a coincidence that the major mental illnesses typically strike people at precisely the times in our life when we begin to turn away from play? Or that once a mental illness is in place playing often stops altogether?
Playing with our patients should not be looked upon with disdain. In Winnicott's view therapy and helping others are among the most advanced forms of human play. Many professionals feel that it's an honor to be able to play with these people.
More relaxed, equal, and playful relationships with our patients. Long term relationships with people that we come to know, understand and perhaps even share environments with. A shift from being in charge of people to consulting with them about strategies for getting the best out of their individual brains, and developing the most satisfying lives possible. Recognizing that each person is ultimately responsible for his own life and his own behavior. Working to provide better environments and specifically tailor them to meet the needs of the client. These are the directions that the psychiatric profession may take into the future. The trajectory that we've been on so far hasn't been that good for us, our patients, or our society.
Psychiatrists of the future
It's strange to think that the field of psychiatry as we've come to know it will only exist in this form for a very short time. We've only been around for a hundred years or so and we're already turning into something very different than the way we started out.
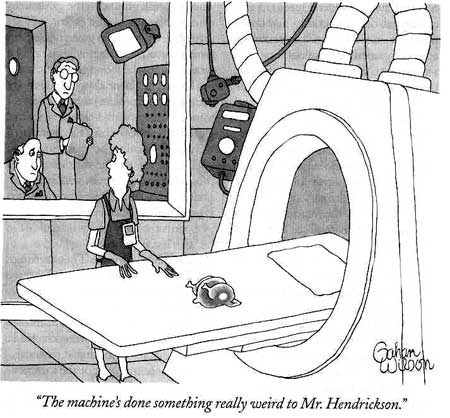
It won't be long now - maybe less than a decade - before machines will determine psychiatric diagnoses. They'll tell us exactly what parts of the brain are malfunctioning and whether a particular gene sequence is involved. Choices about medications and dosages will be machine made too. The way that our bodies will respond to a medication will be determined before we take it.
So where does this leave us shrinks? Many of us aren't technologically inclined. And coming to work to run patients through elaborate computerized instruments won't be that interesting anyway.
Ironically, the machines may prove to be our salvation.
When the technology gets good enough to demonstrate which treatment approaches are truly most effective for people with severe mental illnesses those treatments will certainly become more sophisticated and widely embraced. The importance of factors like nutrition, activities, and good environments will become apparent. The value of supportive relationships, laughter, and improved self-esteem on brain functioning will be recognized. Psychotherapy will be seen as a biological treatment.
The importance of considering the whole person and their entire environment will become too obvious to ignore. The "holistic" approach won't be embraced because it's hip or trendy. We'll use it because to do otherwise will be proven to be less effective.
This bodes well for our field. There will be room for all sorts of talents in tomorrow's psychiatry. Technology, brain research, and creating new medicines will coexist with psychotherapeutic understanding, education, and environmental engineering. As we become more sophisticated in our ability to comprehend the human condition we'll draw more gifted, curious, and humane professionals into the profession.
Maybe this is a good time to be a psychiatrist.