Readings in Humanistic Psychiatry
Defining the problem
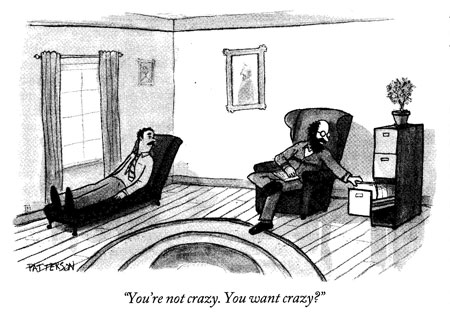
Dealing with insanity is far more interesting than most people would imagine. Consider a few examples.
Going to sleep was terrifying for Samantha. She was convinced that she grew extra appendages on her back each night but they were cut off by a creature that lived in her mattress. He then sold them to local fast food restaurants. "Every time I pass a Wendy's I just shudder", she exclaimed.
Stella believed that she and her psychiatrist had coexisted as disembodied heads on the tongue of a giant polar bear for the 60 years prior to her hospitalization. Dangerous white bears were everywhere in her world, even living in deep pits below the ground. She once explained how she had fallen into one of those holes. The polar bears were packed in so tightly that they had to stand upright. She could only move around by walking on top of their heads.
Gene was absolutely certain that someone was tracking his whereabouts with "depth finders" of the kind used for fishing. His tormenters followed him everywhere, for the sole purpose of using television remotes to cause a tickling sensation in his rectum.
When trainees encounter stories like these a sequence of reactions often occurs. At first they may protest that no one could actually believe things that are this strange. They may even conclude that the patients are putting them on. But Samantha had lived in a state hospital for eight years because she was too terrified to leave. Stella was carrying firearms to protect herself from the dreaded bears. And Gene had actually fired a shotgun at a neighbor who he thought was tickling his privates.
After it becomes apparent that people can truly live in worlds that are this uniquely bizarre, the students may become involved in trying to understand the meaning behind the odd beliefs. Every psychotic symptom reveals, at some level, the wishes, beliefs, and fears of the individual. Helping psychotic people to become more understanding and tolerant of themselves used to make for fascinating careers in the days before our powerful antipsychotic drugs.
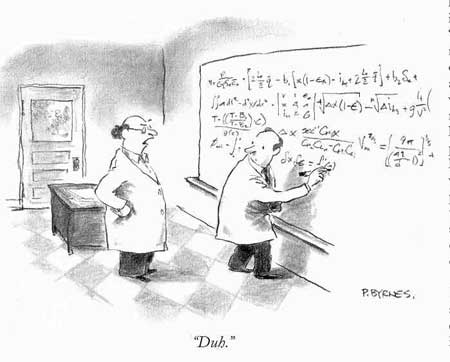
After a seasoned clinician hears stories like these for years on end some underlying patterns begin to emerge. We get less caught up in the details of the crazy ideas and begin to focus on the mental mechanisms that are behind them. As the commonalities in our patients become more apparent we may begin to see the same patterns operating in groups of sane people. Organizations can become just as crazy in their own way as any single person can manage.
It may seem incredibly far-fetched to suggest that our country's mental health system is now insane in a manner similar to those three patients. The diagnosis of insanity is never one that should be made lightly. And it's never wise to make any diagnosis before the history is taken and the examination is complete. So we'll put off the formal diagnosis until later. For now, let's consider some troubling symptoms.
The system becomes a patient
One of the first clues to the fact that our complex system of mental health care has gotten goofy lies in the value assigned to human lives. Throughout our country we've essentially taken the position that some human lives are expendable. We sit casually by while the ranks of poor, hopeless, and homeless people expands with each passing year. Some very sick people who suffer disorders that are not of their own making end up trying to survive on as little as $208 per month. Locally, leaders are taking steps to reduce the pool of people receiving even that tiny degree of support.
But what happens when one of those disposable humans threatens to take his own life?
Suddenly the same guy that society cared nothing about is receiving mental health services that can easily exceed $100,000 per year. Threats of suicide trigger liability concerns. Money is no object when it comes to protecting the valuable tails of our helping professionals.
After we spend countless dollars on hospitalizations, drugs, and court hearings we give some of those patients extraordinarily expensive service packages in hopes of preventing further suicidal thoughts. Others are given nothing but a return trip to the poverty and isolation that prompted their thoughts about ending it all in the first place. This is at least a little crazy.
We'll see that our mental health systems spend the first 50 cents of each tax dollar on commodities that mentally ill people never see. Drug company shareholders and career bureaucrats get their cut before the needs of a single patient are even considered.
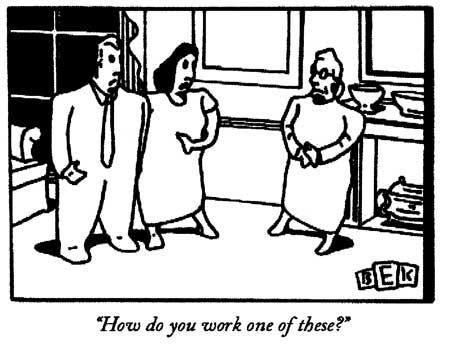
Our intricate meshwork of bureaucracies are run by people that have no contact whatsoever with mentally ill people. They have no way of knowing whether the things they try to accomplish actually work or not. In a very real way the people in charge of the system are out of touch with reality.
How do we decide who will receive help in a system that has nowhere near enough resources to go around? We have more layers of eligibility determination than the uninitiated could possibly imagine. Strangely enough though, it ultimately comes down to what people report is going on in the privacy of their own skulls. Sometimes the reports aren't exactly accurate.
Clients who are clever enough to realize what the professionals need to hear can tap into a rich funding stream of supports. Drug abusers and personality disordered individuals who's lives would be better if they worked may get indefinite public subsidies. Many severely ill people don't think there's anything wrong with them and end up with nothing.
Our system of mental health care is based on outmoded ideas about people receiving treatment that restores them to full functioning. But when individuals do show any evidence of becoming more independent in response to our efforts they may quickly find that the rug has been yanked out from under them. We demand that they show continuing evidence of dependency if they're to receive any help at all.
These are just a few of the presenting symptoms that our enormous patient comes to us with. As the examination progresses many more will become apparent.
How to fix a broken mental health system
The subtitle of this work holds within it two basic assumptions: That our public mental health system is badly broken and that the problem is fixable. Should either of these assumptions prove to be untrue then this book will not amount to much.
Before deciding whether a complex piece of machinery is malfunctioning we have to know what it's supposed to do in the first place. So let's review what a public mental health system would do if it were working properly.
The reason that we have a publicly funded system of mental health care comes out of an awareness that there will always be people in a society that, through no fault of their own, suffer from mental disorders of such severity that they will be unable to care for themselves. Unless we're prepared to allow these citizens to die of neglect or are willing to mandate that families or charitable organizations must assume the burden of caring for them, we have to agree that our tax dollars will fund a basic safety net for mentally ill people.
A net laid upon the ground
So the first function of a public mental health system is to provide that safety net. To make sure that people who cannot reliably provide for themselves are given adequate food, clothing, shelter, and medical care. Even at this most basic level our system is failing miserably. Things may be somewhat better in other parts of the country but here in urban Minneapolis you can't swing a cat without hitting a homeless mentally ill person.

Sadly enough, it would be nice to be able to say that the homeless shelter pictured above is as low as our safety net will allow someone to fall before it catches them. But the only way to get onto one of those 70 sleeping mats -overseen by one untrained volunteer-is to win a lottery that's held each night. On any given night roughly half of the lucky winners will be suffering from a severe mental illness.
Many of our most severely ill patients can't deal with living in conditions like this, even when they hit that jackpot. Problems with crowding, crime, and substance abuse are just too much for their nervous systems to deal with. So they try to fend for themselves outdoors.

Still occupied. Courtesy Patrick Arden Wood
Encouraging the best functioning possible from our clients
Even if we were doing a credible job of providing reliable safety net services we'd still want more from a mental health system. People should be given meaningful incentives and opportunities to move towards recovery and to become as independent in their functioning as their disordered nervous systems will allow. This is another area where we fail these people.
The average person suffering from a disorder such as schizophrenia receives disability income of right around 600 dollars per month to live on. Just surviving on that income would be a real challenge for most of us supposedly healthy folks. The challenge proves insurmountable for many severely mentally ill people. They need a lot more help to get by but the only way to receive more services is to demonstrate that they really need them. Getting hospitalized on a psychiatric ward is the main route to subsidized apartments and in-home supports. But that road is heavily traveled and quite competitive these days.
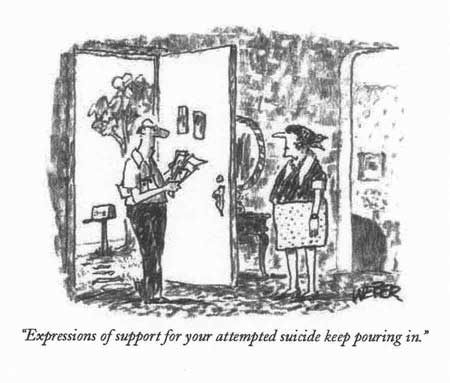
Here in Minnesota's metropolitan area these hospital beds are so scarce that we routinely send patients hundreds of miles to other communities and states when they need treatment. Only clients who appear to be actively dangerous to themselves or others are able to get hospitalized. So our clients must now play a peculiar game with us. They know that they must claim to be suicidal or homicidal to get help. It's well known on the streets that the magic words needed to get admitted to hospitals are "I'm hearing voices telling me to kill myself" so that's what a lot of people say.
Of course there are many people who are that ill but that doesn't change the fact that our system now requires proof of dangerousness as a prerequisite to getting enough help to stay afloat. Not only do we fail in providing incentives to function more independently, we insist that people be severely decompensated - or at least be able to present that way - if they're to have any chance at getting the level of services that they need.
Just about anyone would agree that any client supported with public dollars should be encouraged to function as independently as possible. But again we drop the ball. Studies have demonstrated that "supportive employment" is regarded as one of the best things a mental health system can provide for its clients.
Just about everybody functions better when they're working but severely mentally ill people have tremendous difficulty with competitive employment. Studies find that 85-90 % of people with severe mental illnesses are unemployed. The research evidence confirms that they often need special settings and supports to work. But we've actually decreased opportunities for supported employment here. Clinical evidence always takes a back seat to financial realities. If we can't get someone else to pay for services like specialized work settings we're not going to provide them.
Making the best possible use of our tax dollars
This brings up another important function that we should be able to expect from public mental health systems. Since the services are paid for through taxes levied on people that work hard just to support their own families every effort should be made to spend these dollars in the most efficient and economical way possible.
Nowhere are our failings greater than in the area of efficient use of the taxpayer dollar. At least 30 per cent of our mental health budget goes right to supporting our large bureaucracies. Local, State, and Federal agencies engage in a constant battle to make the other agencies responsible for the care of mentally ill people. In Minnesota this struggle has reached bizarre proportions.
Our top State mental health officials recently managed to slip a new law through the legislature without a word of public discussion. This law reclassified all adult mental health services as "enterprise" based. This means that all programs for mentally ill adults must now pay their own way by generating billings. Of course since almost none of our patients work at jobs that provide health insurance, the only payer that can pick up the tab for these bills is the Federal government.
The Federal health care programs are on the verge of collapse. And small wonder.
Officials of local programs that won't cough up ten dollars for a client out of their own budgets will cheerfully approve service packages for the same person that may run 10,000 dollars per month or more - as long as the money comes from the feds. This may seem like an exaggeration but, unfortunately, it's all too true.
The programs now offered to Minnesota's mentally ill adults weren't even in existence just five years ago. Assertive Community Treatment teams, Intensive Residential Treatment facilities, Community Alternatives for Disabled Individuals, Corporate Adult Foster Care, and round-the clock "Personal Care Attendants" are available to a fortunate minority of our clients. All of these programs have a couple things in common. Yearly tabs for an individual's services run at least 60,000 dollars on average. And the services provided are the ones that can be cost-shifted to Federal programs.

We're currently in the process of selling off beautiful old State Hospital campuses and replacing them with a much smaller system of 16 bed hospitals, despite the enormous pressure for psychiatric beds. Bureaucrats strive mightily to spin this movement as an effort to "have patients treated closer to their homes" but the truth is that if a psychiatric facility is larger than 16 beds it's classified as an " Institute for Mental Disease" and the State has to pick up the tab. 16 beds or less and we can bill the Feds.
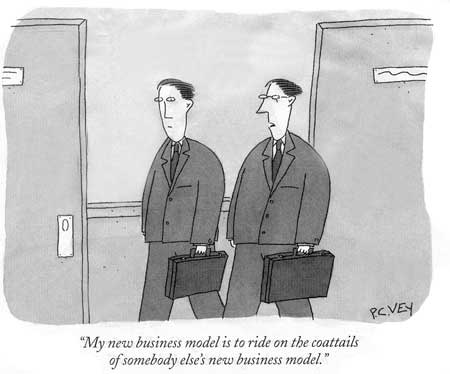
Of course the federal bureaucrats don't sit quietly as costs are shifted to them. They respond with an ever increasing array of rules, regulations, eligibility requirements, and reviews in order to protect their own budgets. The net result is an ever increasing push to expand the bureaucracy that deals with all of these paperwork requirements, with less and less available to trickle down to the actual people that the system was supposed to help in the first place.
After the first 30% of our tax dollar goes to these competing, politically charged bureaucracies we then siphon off the next 20% or so to the for-profit pharmaceutical companies. Billions upon billions of dollars are involved. Pills that cost a penny or two to manufacture can cost the taxpayer ten bucks or more. And the drug companies have been ramping up the prices for their products for the past several years in preparation for the weirdly complex and hideously expensive new Medicare drug plan.
Much of the money we spend for the medications that our patients need goes to stockholders in pharmaceutical companies. Then we have to pay for all of the lobbyists who're paid to keep the golden goose of drug company profits alive in America. A few dollars seem to eventually find their way into the campaign funds of our politicians. Doctors are lobbied too. There is now one drug company representative for every eight physicians in our country and they're always out promoting the idea that their new products represent real advances in treatment- even where such claims are patently untrue.
It's easy to complain about the outrageous profits brought in by the drug companies, and the sleazy tactics that they use to maximize them, but criticizing for-profit corporations for trying to increase revenues is a lot like bringing a horse in to your home to live, then complaining when the carpets are soiled. These companies exist to make as much money as possible-usually at the expense of the taxpayer-and to think they'd behave otherwise is naive. So is thinking that the situation will change by itself.
A mental health system that is truly devoted to providing the best possible quality of life for its clients at the lowest possible cost to society will obviously not be able to continue giving the first fifty cents out of every dollar to support people that don't even have mental illnesses. Bureaucracies will have to be streamlined dramatically. An enlightened government would actually manufacture and distribute these medications itself beginning the day that patents expire on them, rather than continue to pay mark ups that can easily exceed 1000% per pill.
A serious look at the literature on the effectiveness of these medications will reveal that the newest, most expensive medications are really no more effective in reducing the symptoms of mental illness than the medications that we had decades ago- no matter what the glossy drug advertisements would have us believe. The newer drugs typically have better side effect profiles but even that comes into question the longer they're on the market. And the majority of medications that are the backbone of today's mental health treatment will come off patent within the next couple of years.
Distributing our limited resources fairly
In a logical mental health system the sickest patients- the ones least able to care for themselves- would receive priority when goods and services are doled out. Once again our current system comes up far short of expectations.
The costs for a decent mainstream apartment with an enriched program of supports brought in are so prohibitively high that our society simply can't provide that level of care to everyone that could benefit from it. So a small minority of our clients receive Cadillac-level services while the rest are left battling for crumbs. Human nature being what it is, it's not too hard to predict who will get the bulk of the resources. The severity of one's illness doesn't receive much weight in the decision.

Patients that carry large costs to the agency in charge of distributing the services will always receive priority. People who have a fondness for psychiatric hospitals and are clever enough to access them will always have access to the best community services. Someone will figure that even that 10,000 dollar per month group home is still cheaper than a 15,000-30,000 dollar per month hospital bill. Whether or not we're providing incentives for the person to be troublesome or non-compliant with treatment isn't a consideration.
One of the common symptoms of severe mental illnesses is a steadfast belief that the world owes us something that we're not getting. Some patients essentially view themselves as the center of the universe and expect to be treated accordingly.
Many of these people have the time and energy to relentlessly campaign for a larger slice of the pie. Whatever they're currently being given is not enough. When they complain to administrators their complaints are typically taken at face value. Oftentimes it's easier to meet the patient's demands for more services than to go through the process of determining that the current benefit package is adequate. And the client that's savvy enough to go up the organizational ladder with his demands is very likely to be successful. No administrator wants to be in the position of explaining to his supervisor why this poor client's needs weren't met.
Sometimes it's parents or other interested parties that push for enriched services for the client. Having a politically active family member may be the surest route to that subsidized apartment with lots of supports. Once again though, it's not how ill you are that really matters. Quiet, isolated patients with no one to advocate for them fall easily through the gaping holes in our safety net. If they happen to be members of a minority race or an immigrant group it's even less likely that they'll receive the help that they need.
Identifying preventable causes of mental illness
An ideal mental health system would be able to act in ways that would decrease the number people in society that are suffering from mental illnesses to the fullest extent possible. Illnesses that are preventable would be identified and dealt with early on. Where the disorders spring from genetic or prenatal factors treatment would be offered to keep the illnesses from progressing to their most severe forms. If there are factors in our society that lead to a greater incidence of mental illnesses we'd seek them out and try to minimize them. Of course these lofty goals are far beyond the reach of our overburdened system of mental health care.
These days appointments with public sector psychiatrists tend to run for 10 -15 minutes, every three to six months. The visits are typically centered entirely around making adjustments in medications. Efforts to understand the person's life situation or discuss non-medication alternatives rarely show up on the agenda. It's often difficult enough for the doctor to even remember who the patients are much less concern themselves with preventive care.
Most of the research into the treatment of mental illnesses is funded through pharmaceutical companies. So are most of the educational conferences and the shrinks who speak at them. So some very important questions about mental illness are unlikely to be addressed at all.
It used to be said that one in every four adults will have a diagnosable mental illness at some point in their lifetime. Latest estimates suggest that that figure may now be around one in two. Something powerful and important appears to be going on in our society that's predisposing our citizens to mental illness. But so far we've been unable to do much to address this issue beyond attempts to provide greater amounts of increasingly expensive medications to people once the disorders have taken hold.
"Evidence Based Practices" to the rescue?
If you can find a mental health administrator who's bold or foolhardy enough to publicly admit that our mental health system is in shambles their very next sentence is likely to include the words "Evidence Based Practices". This concept is held up as the long awaited light at the end of the tunnel throughout our immense bureaucracies.
Anyone unfortunate enough to regularly attend mental health planning meetings has witnessed a strange ritual. Most of the policy makers have no experience in treating mentally ill people, or they may have worked in the field decades ago when things looked very different. The one concept that the bureaucrats have all managed to grasp is that any system fixes on the horizon will have to come out of the "Best Practices" literature. Of course there's a reason for this.
The idea that treatments should be directed by the best clinical evidence available is such common sense- and so difficult to criticize- that anyone can feel safe in the knowledge that comments along these lines will be met with solemn nods of agreement. Those kinds of nods are highly valued. But the actual findings and implications of the Evidence Based Practice literature are given scant attention.
There are now six areas of mental health care that have achieved the exalted status of "Best Practices" for mentally ill people: Supportive employment. Family psychoeducation. Assertive Community Treatment. Integrated treatment for people with both mental illness and chemical dependency issues. Illness Management and Recovery. And algorithm based medication guidelines. There is no objection whatsoever to any of these areas here. But let's pause for a moment to consider what these efforts to distill all of the best research available into guidelines for mental health system development really tell us so far.
The idea of supportive employment was already mentioned. It basically finds that it's very hard for severely mentally ill people to find and hold mainstream jobs. They typically require specialized settings, approaches, expectations, and supports if they're to work regularly. And work is very important for their mental health.
Family psychoeducation is not mysterious. It shows that teaching people and their families about the nature of mental illness, strategies and benefits of treatment, and ways to manage symptoms are extremely helpful. It's quite consistent with some older literature that demonstrated that people with disorders like schizophrenia may be uniquely sensitive to criticism from their loved ones and that more informed and tolerant relationships may reduce the frequency of breakdowns.
Assertive Community Treatment has shown us that it makes more sense to bring mental health services to people where they live than to keep moving them to very expensive treatment facilities based on fluctuations in their clinical condition. ACT also suggests that having several professionals from a team know the clients and be able to deal with their problems is better than having just a single person involved.
Integrated "Dual Diagnosis" treatment finds that providing mental health and chemical dependency services in a coordinated way works better than making clients deal with two very separate care delivery systems at the same time.
Illness Management and Recovery tells us that it's useful to systematically teach patients about their illness, its symptoms and strategies for managing them.
The findings of Evidence Based Medication Treatment can seem a little more complex but when you boil them down they look like this: In the treatment of any of the major mental disorders there are almost always a number of medications that are equally effective. There is currently no way of knowing exactly which patient will respond to which medication. It makes sense, then, to use trials of single medications- with careful attention to target symptoms and side effects- for most people in most situations. If a particular medication doesn't work another trial of a different medication should follow. People should probably have at least several trials of single medications before moving on to more complex, multiple drug regimens.
It's probably obvious that all of these findings that are now felt to have sufficient "evidence" behind them are pretty much common sense. In fact a seasoned clinician could have most likely predicted all of these results based on experience alone.
Just because something is consistent with common sense doesn't mean it should be ignored (despite prevailing practices). But to think that the new mental health system that we so desperately need could be built on these six areas of accepted evidence is just nonsense. We need answers to a lot more questions but when the many efforts to summarize the best clinical evidence are reviewed it becomes painfully apparent that almost all of the important questions have "insufficient evidence to make recommendations".
Even questions as basic as whether case management services for mentally ill people are worthwhile have too little research support to answer. We don't know what treatment for most of the mental disorders should really look like. There's a paucity of information about combining multiple medications in the treatment of any mental illness. And perhaps the single most important question facing us as we try to develop new ways of caring for people in the community has been subjected to almost no decent research.
Look at what the Cochrane Group concluded about the problem of providing supportive housing to these people:
Many people with serious mental illnesses need support living in the community. For some people this takes the form of supported housing. In this review we looked for the best evidence for the effects of this type of housing - and found none. Whether or not the benefits outweigh the risks are currently only a matter of opinion, debate and informal reports. Well-designed, conducted and reported randomised trials are needed in this area.
The Cochrane Database of Systematic Reviews 2005 Issue 4 Copyright © 2005 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Of course, there's nothing at all that's wrong with the efforts of the professionals who are trying so hard to review the quality and implications of all the available literature on an enormous variety of clinical questions. The objectivity that they bring to our field is a welcome relief from so many decades of conjecture and opinion. The problem comes when administrations try to grasp at the few straws of decent evidence to build a new mental health system with them.
A careful examination reveals that even those six areas of established evidence receive very little more than lip service when planning takes place. We're quick to grab on to an area or two that we can get another agency to fund, then add stringent "fidelity requirements" until both clinicians and clients feel handcuffed. The Evidence Based Practices that we can't get funded through the Federal budget are conveniently ignored. And trying to establish innovative programs that actually seek to answer some of the hard questions - and add to the needed "evidence"- is beyond the scope of anything that our bureaucracies will consider.
So if you should happen to be in a meeting where someone says how wonderful things are going to be for our mentally ill people as soon as we get our "Evidence Based Practices" into place it's probably best to just nod. And feeling solemn shouldn't be too difficult to manage.
Is our mental health system really fixable?
It's easy to criticize our exiting system of mental health care. Some of us have made careers of it. But offering realistic, testable hypotheses about how to get out of this mess is another matter entirely.

The remainder of this work will focus on concrete things that we can do to make our public mental health system better. No one is saying that it will be easy. We'll have to start with a different understanding of what it actually means to be mentally ill. We'll also have to rethink our existing ideas about what recovery from these disorders entails. An honest look at the way our society is changing - particularly in regard to how we raise our children - will be necessary.
We'll try to understand exactly what environmental factors need to be altered in order for these people's malformed brains to function at their best. Some basic principles that we can build a new system of mental health care upon will be laid out. Several simple residential models aimed at providing the things that mentally ill people really need, in the most integrated, cost-effective, and humane manner possible will be proposed. A new look at the way we provide incentives and consequences to these clients - and the behaviors that we really want to shape - will be offered. Finally, the barriers to system change that will have to be overcome will be addressed.

When you deal with providers and other people intimately familiar with our mental health system the idea that our current system of care is broken is taken as a given. But hope and optimism about things getting better are in very short supply. We often seem resigned to the fact that things will continue to deteriorate for our expanding pool of people with severe mental illnesses. The idea that we'd be able to simply replace the existing care delivery system with a new and better one is attractive but just seems too far-fetched to even consider.
Sometimes when we see a complex problem in a new way solutions become apparent that we were previously blinded to.
Building testable model programs on a small scale, then reproducing them if they work, is clearly within our reach. The current mental health system has enough dollars devoted to it for us to provide a decent quality of life for every client that we serve, if only we use our resources more wisely. At least we'd better hope that this is the case. If we continue on our present course the implications for our society are too dreadful to consider. The mental health system that we have fifty years from now simply cannot look like the one that's currently in place.
There is certainly an enormous task before us. Building a truly improved mental health system will require a thoughtful, integrated approach and a commitment to systematically exploring new ways of providing our societal safety net. But if we can fix the problem we're facing here we can fix anything.