Readings in Humanistic Psychiatry
Disincentives to System Change
Just about anyone who's familiar with America's public mental health system will tell you, at least privately, that the whole thing is a train wreck. We've created something so cumbersome, complex, and expensive that it's almost an accident when people with severe mental illnesses do receive good care.
If we had the chance to really design a new system of care, using all of the information that we've accumulated over the recent decades, it would almost certainly bear little resemblance to the one that we have now.
On the surface it would seem that improving our system should be pretty easy. We could begin by building a new and improved version, as close to ideal as we could make it, alongside our existing system. Then, as we could demonstrate that the new system was doing a better job at a lower cost, we could shift resources to it over time. Kind of like tapering off someone's clozapine while they're being started on Abilify.
The Model Community Programs outlined earlier would be a nice place to start our efforts to revamp the whole system but there are other models out there that we could use instead. And as has been repeatedly emphasized, it's really the commitment to a process of improving our system that's important rather than the specific models that have been offered.
Anyone that might decide to go forward with this common sense approach in his local mental health system should be prepared for massive resistance though. It's unlikely to be direct opposition that will be encountered. People may nod and smile and say what a good idea you have. There may even be committees set up to explore the idea of moving forward in whatever bold new direction has been suggested. But nothing will really change at all.
The resistance may be so subtle that that you can't even tell where it's coming from but you can count on the fact that there will be resistance and that it will be extremely effective.
The Soteria Project
If this view of our system's reluctance to make changes - no matter how good the options that are being put on the table - seems a little too cynical a quick review of the outcome of another humane and common sense project is worthwhile.
Back in the late 1960's there was a respected psychiatrist named Loren Mosher who headed the Center for Schizophrenia Studies at the National Institute of Mental Health. Dr. Mosher decided to try a nice experiment. He created a home where people with schizophrenia could be treated by simply providing a decent, caring environment for them. The staff were not trained in the mental health disciplines but were selected for just being caring, empathic people who would treat the patients with kindness. Antipsychotic medications weren't a part of the treatment. Outcome measures were set up to see how simply providing a good home to live in would measure up against conventional psychiatric treatments that emphasized correction of those "chemical imbalances".
It won't be possible to do justice to the project in this space (more details are available here) but we can skip to the punch line. The patients who lived at Soteria House, and several others like it that followed in the United States, Scandinavia, and Switzerland had outcomes that were every bit as good as the people who were treated with the drugs.
A person might think that demonstrating the importance of providing decent living environments for people with schizophrenia to have a chance at recovering in would have resulted in the creation of lots of houses like that. But such a person would, obviously, be unfamiliar with the way our mental health system works. Instead of our government's embracing the work of the Soteria Project, Dr. Mosher was essentially drummed out of the NIMH. Funding was progressively cut off for his project until it was no longer possible to operate the houses.
Perhaps Dr. Mosher's error was in creating a system that challenged the conventional wisdom of using medications to reduce psychotic symptoms. Even some of us who were trained in treating psychotic people without medications are still convinced that the antipsychotic medications have a valuable place in our treatment of schizophrenia.
Drawing battle lines over that issue is likely to get any psychiatrist seen as a dangerous crackpot who must be excluded from the shrink club at all costs. But it's hard to ignore the fact that the Soteria Project and others like it have demonstrated that providing safe, homey, living environments in which people with schizophrenia are treated with kindness and understanding can go a long way towards helping them to recover.
The other lesson to be learned from the project is, of course, that just because an idea makes sense there is no guarantee that it will have any chance of being implemented in our mental health system.
Where does the resistance to change come from?
Whenever one sees something as goofy and dysfunctional as our current mental health system being perpetuated for decades on end - in the face of numerous attempts to change it - it can be safely assumed that there must be people somewhere who benefit from keeping things the way they are. Of course those people may not acknowledge the fact - even to themselves - that they stand as an impediment to change. But there are a lot of people who would have something to lose if we could suddenly change our system of care to one that actually made sense for the people it's intended to serve.
Strangely enough, some of the patients in our system would be unlikely to advocate for changes in it. It's been estimated that in our programs that are set up to help homeless people around 90% of the resources go to 10% of the clients. That figure would be a bit excessive for our mental health system at large but the principle still applies. An awful lot of resources go to a relatively small fraction of mentally ill people. If you're one of the lucky few that gets a nice subsidized apartment, in-home psychiatric and nursing care, a homemaker, and round the clock "Personal Care Attendant" time it's unlikely that you'll be picketing your local mental health center.
Those patients certainly do exist in our mental health system but how ill you really are has little to do with whether you'll get those kinds of services. In fact one probably has a much better chance of accessing that sort of help if they have a personality disorder or a milder version of the major illnesses. Having an active and involved family member advocating for you or a case manager who is energetic and talented will also increase the likelihood of your getting the Cadillac version of a support system rather than the broken down scooter that so many people end up with.

Some of the opposition to change comes from individuals who aren't even connected or familiar with our mental health systems.
From the standpoint of some people all systems that are designed to care for disadvantaged people qualify as "charity". If you're working two jobs to make ends meet the idea that some of your income should go to help support people who aren't working - for whatever reason - can be pretty distasteful. And it's increasingly common to see people build a political career by talking about "all the freeloaders that are taking advantage of the hardworking taxpayers of this country". Our society is becoming increasingly divided - and some would say cold hearted - when it comes to using tax dollars to assist other people who are less fortunate than us. In fact some even hold the view that it's the people who receive the entitlements that are the more fortunate. And there's no getting around the fact that in our present social system there are people who receive entitlements when they could be working. So any talk of taking better care of mentally ill people will be sure to encounter arguments from people who just don't want to take care of them at all.
The problems always become clearer at the edges or extremes. What should our society do about someone who was hit by a drunk driver and, through no fault of their own, ended up a quadriplegic? Are we prepared to tell that person that if they can't work or take care of themselves that society will leave them to perish?
While we're rapidly becoming a country that views some human lives as disposable, problems come when we have to decide how to actually do the disposing. Is there anyone that would really advocate for taking that brain-injured person out into the woods and leaving him to die? Or for euthanizing him against his will?
The situation is not that different for people with severe mental illnesses. They, too, have brain problems that were not of their choosing. Asking some of them to support themselves via full time employment can be just as unrealistic. There will always be some people that just about everyone will agree deserve some help in living. But what that help should look like is another question.
The issue of where the lines should be drawn is another important one. There's always the tendency to say "we're going to drastically cut back the number of people who will receive assistance from society. People are going to be required to be self-sufficient now". But if we draw the circle in too tightly we still have to decide what to do with those that we're not going to offer help to.
If our idea is that people will work in minimum wage service jobs that don't give them a chance of having a decent place to live, medical insurance, or any real opportunities for advancement it shouldn't be a surprise when they flood our social programs. If they can have better housing, medical care, and services by not working than they can through employment they'll do or say whatever is necessary to get through the door to those social programs. That's just the way it is whether we agree with it or not.
Our society is quick to tell people that they should "pick themselves up by their bootstraps" but that's pretty hard to do when you're standing knee deep in muck.
Non-specific resistance to change
Of course the very idea of change is likely to elicit some common reactions in any of us. We're likely to become defensive right away. Some form of "what's wrong with the way we've been doing it?" is likely to be encountered. People may readily feel that their previous efforts to help have been devalued or discounted.
The known always feels safer than the unknown too, even when the known isn't all that great. "What if the changes endanger my job or my benefits?" What if too much will be expected of me in the new system?" What if there are hidden strings or agendas attached to these changes?" What if people find out that I haven't been doing valuable work after all?" "What guarantees are there that the changes will make things better - what if they actually get worse?" "Look what happened the last time that they tried to make changes - we're still recovering from that."
Some version of these complaints will be encountered whenever any change is proposed, no matter how much the changes are needed or how well thought out the proposals are.
Human nervous systems are intricately attuned to changes in the world around us. The slightest motion, sound, or even a difference in air temperature is likely to capture our attention. Our survival once depended on sensing minute changes in the environment and being able to adapt accordingly. So it's no surprise that changes of just about any kind would result in an activation of that "Amygdala" system, with all of its tendencies to activate us or prepare us for battle.
Could psychiatrists stand in the way of change too?
It's odd to even think that we psychiatrists might be presenting obstacles to changes that could improve the lives of our patients. But that does happen in our current system, for a variety of reasons.
A prominent local psychiatrist is always opposed to any programs aimed at improving the lives of mentally ill patients in the community simply because he wants to make sure that the beds in his hospital wards are filled at all times. Maximizing the revenues coming into his department is what it's all about for him and he doesn't believe that there is anything ethically wrong with that. One hopes that primates of that developmental level aren't encountered elsewhere in America.
Usually the resistance that we shrinks might feel towards system change is rooted in more subtle motivations. Anyone who has had the nerve-wrenching experience of being around a lot of psychiatrists is likely to tell you that for the most part we really aren't bad people. We tend to be pretty curious about human nature, most of us can be kind if you catch us on a good day, and we typically take our responsibilities to the people we care for very seriously.
Our objections to sweeping reforms of the mental health system commonly come from the very things that we see happen when we try to help our patients.
One of the many peculiar things about being a psychiatrist is that we can prescribe a list of medications that costs literally thousands of dollars per month for our patients and no one blinks an eye. After all, these are treatments that have been ordered by a physician so who is going to question their expense or appropriateness? But if we were to order a specially designed living environment that would provide the patient with his best chance at recovery no one would fill that prescription, even if it cost just a fraction of what the drugs do.
So we're often in the position of prescribing medications for people who live in terrible environments in which they're exposed to chronic stress, stigma, and social isolation. And our patients do benefit from our medications. We see that with our own eyes all of the time. People do become calmer when we give them major tranquilizers or use antidepressants to decrease the connections between their thoughts and emotions. And they certainly do tend to decompensate or become less stable when they stop taking those medications.
When we see people improve in response to our treatments it becomes very hard to question whether those treatments are worthwhile, especially when we have so little else to offer them.
If we didn't think that providing medications to our mentally ill people was helpful most of us couldn't come to work to do what we do each day. Plus we typically have little confidence that the administrations that we work for could actually set out to make improvements in our system of care without bungling the whole job entirely.
The biggest obstacle of all

Nothing stands in the way of significant changes in our social programs like these shadowy figures do. Our mental health systems aren't actually built on an infrastructure of affordable housing units or community support teams. Instead we've invested our tax dollars in structures that look like this. Of course the main problem with these structures is that they're really hard to sleep in.
All of the programs aimed at serving the mentally ill throughout the federal government, states, counties, hospitals, and non-profit corporations have their own organizational hierarchies of this nature. The one pictured above isn't even particularly complicated or dense compared to many. Each little box may also sit at the top of its own hierarchical ladder. And each agency has to interact with countless other agencies of a similar nature, even though they may not speak the same language or share the same motivations.
Every agency has its own organizational chart and our mental health systems contain more agencies than one could possibly imagine.
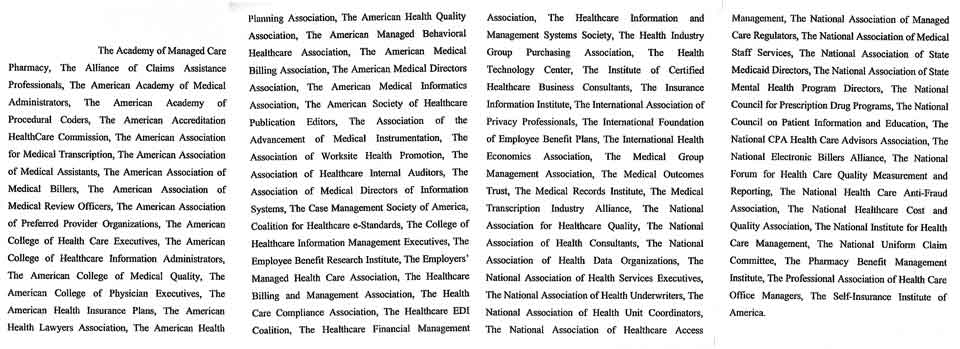
Minnesota's Attorney General's Office compiled this list of organizations that represent some of those bureaucracies involved in our health care system.

Where a person stands in his organizational structure assumes prime importance. What the guy in the box above you thinks and how many boxes you have below you are the real motivators in these systems. Even simple decisions have to "be sent up" to the higher committees for review. Nobody ever makes decisions on their own. There always have to be committee meetings held about everything.
When it comes time to schedule those meetings no one wants it to look like they have too much free time to choose from. Even people who have nothing whatsoever on their calendars may put off meetings, saying "No, I'm all booked up that week". This really does happen. Creating the illusion that one is very busy doing important things is a task of enormous magnitude in these bureaucracies.

Finding out exactly who's responsible for anything may be impossible in these organizations. They're built in ways that ensure that no individual can be blamed if things don't work out. But it's fun to watch the bureaucrats scurry for position if it looks like there will be praise or rewards offered up.
Administrators build careers by making a case for how well they're currently doing things. Any successes must be emphasized repeatedly - and may even be exaggerated on occasion. Of course, many people have benefited from our current housing system, with its emphasis on scattered-site apartments and very expensive supports. It makes sense that those successes would be emphasized. Pointing to the people that one's program hasn't helped or advocating for any changes in this system may be politically unwise.

Convincing any group of bureaucrats to take a chance on something new is a difficult proposition regardless of how eagerly they may try to portray themselves as bold innovators. Existing funding streams for supportive housing, or anything else in our mental health system for that matter, are almost always aimed at replicating models that already exist - regardless of their deficiencies.
There's a tremendous emphasis in our current bureaucracies on using spending streams that spring from a different agency. If they can't find another agency to shift costs to they'll resort to having a later version of their own agency be responsible. Watching the federal, state, and county governments jockey back and forth about who is going to have to pay for what looks an awful lot like a nasty game of "mentally ill tag". This situation is unlikely to change in our lifetimes unless something drastic is done to address it.
Of course which pot of money ultimately funds a client's care doesn't matter much to taxpayers. It's our pockets that the money comes out of regardless of which agency eventually doles it out.
New endeavors must always carry the risk of failure and failure has tremendous implications in organizational trees. There is always that "Peter Principle" to contend with. The "Peter Principle" holds, of course, that in any organization an individual will rise until he reaches a level at which he is incompetent. So everybody in these structures is watching everybody else to see who is now in a job that they're not qualified for.
People plot and scheme for years about how they'll be able to move up in the hierarchy, and at whose expense. The first whiff of the smell of failure sends the underlings into a feeding frenzy.
Organizations try to deal with this very real phenomenon by talking about how important it is to take chances, how their administration is more progressive than others, and how different things are now than they used to be, but nothing really changes. The inertia that is built into these large bureaucracies is truly mind-boggling.
It's not like the administrators that work in these organizations are bad people or don't have good intentions (besides, it's hard to be too critical of any club of which one is a member). Most of the humans that work in these large agencies are pleasant enough and many of them would like to see things get better for the clients that we serve. If you get us in the right setting we'll often tell jokes or stories about how dysfunctional our agencies really are and how impossible it is to change them. Making fun of competing agencies is an even more popular pastime.
The problem is that human nature drives all of us to be primarily concerned with our own status and security within our groupings. Our evolutionary history as primates that live in troops is never more apparent than in established hierarchies like these.

So it's a very legitimate question to ask whether any real system change can ever result from the activities that take place in these large bureaucracies. Their very make up prevents them from seeing themselves clearly enough to recognize or admit to problems within the system. There is always massive inertia that opposes change in any direction whatsoever. And when the changes might involve the very hierarchy itself change is actively discouraged.
Shifting resources from a system dependent on dense organizational hierarchies to more cost-effective ways of providing a good quality of life for clients just isn't much of a consideration when your job depends on being in charge of a dense organizational hierarchy.
The higher one rises in an organizational chart the less likely it is that he'll be in touch with messy things like the needs of actual patients. The leaders of our large State and Federal mental health bureaucracies have almost never worked in positions that involved caring for mentally ill people. The top jobs go to political appointees so it's no surprise when the motivations are ultimately political rather than clinical. And one of the basic rules of group theory is that groups take on the characteristics of their leaders.
It's been argued throughout this book that the single most effective thing that could be done to remedy the problems inherent in these large mental health bureaucracies would be to simply require that every person who works in them has to spend a small percentage of their time working in direct contact with people that suffer from mental illnesses. This would give them some perspective on what's really at stake as they try to decide how our shrinking tax dollars should be spent. It might add a little to our pool of workers that help these people too. But, obviously, this is not going to happen. People might smile and agree that even an idea that far-fetched has a lot of merit but there will be no perceptible movement in the system. Even when glaciers are moving at their fastest you still can't actually see them move at all.
Moral arguments in favor of change are almost certainly doomed to fail. We humans are generally open to arguments based on morals or ethics right up to the point where it might cost us something, then everything starts to look very different. That is certainly the case when it comes to improving the lives of the severely mentally ill people in this culture.
The one reason that we should overcome all of these formidable obstacles to change is that things will be better for us if we do. Our tax dollars will go more directly to the people that need our help. We won't have to spend so much of our money on courts, prisons, and ineffective social programs. People won't be tripping over homeless mentally ill people in our large urban areas. And, most importantly, we'll be able to see ourselves in a new light too.
Anyone that's visited some of those dreaded Scandinavian countries where everyone has access to a good quality of life can tell you that just about everybody seems happier and more secure there - not just the people who are on the receiving end of the social programs. People feel better about themselves when they know that their culture holds human lives as valuable.