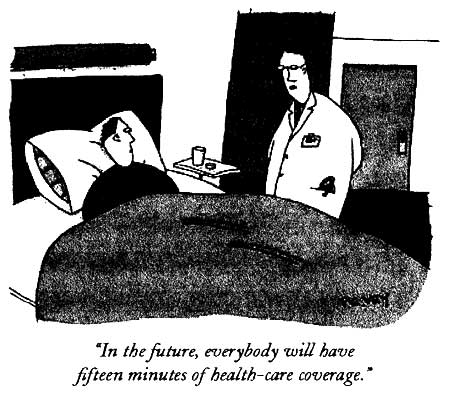
Readings in Humanistic Psychiatry
Where did the "Deinstitutionalization Movement" take us?
The problem of providing adequate community care for our mentally ill citizens isn't new. It has been with us since the very onset of deinstitutionalization, despite the best efforts of several generations of mental health professionals. In many ways this situation is getting worse with time and the trend is likely to continue unless we find new ways of understanding and approaching this profound social issue.

State Hospital Ward circa 1950's
The movement to relocate patients from large State Hospitals back into their communities began back in the early 1960's. Changes in civil rights legislation and the introduction of more effective medications converged, resulting in a massive movement of mentally ill people. It seemed like the most humane thing to do at the time.
In retrospect we can see that this decision, however well-intended, left many people in far worse conditions than they had endured back in the asylums. When discharged from the large institutions homelessness, poverty, inadequate treatment, stigma, and social isolation awaited far too many of them.
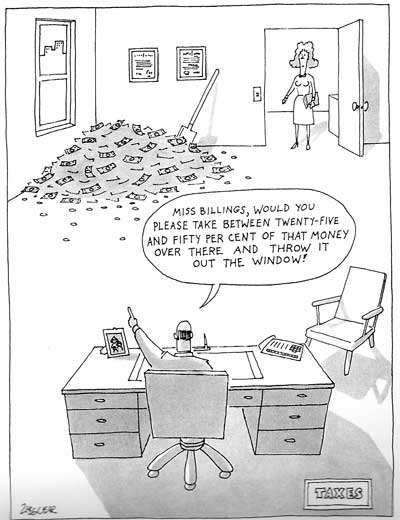
Decades later we're still stuck with a mental health system that's grossly inadequate for the task at hand. It's hideously expensive. Waste and inefficiency are constants. Dignified treatment and personal choice are in short supply. The things that the recipients of these programs actually need are rarely provided. More money is spent determining eligibility than on food and shelter. Relieving the emotional suffering of humans with brain problems has become a source of enormous profit for some people but the money isn't translating into better lives for those we're supposed to be helping.
If we were to build a new safety net for mentally ill people from scratch the one thing that's certain is that it would bear little resemblance to the one we have today.
There is much to be learned from nearly a half century of failed attempts to provide a meaningful safety net for our mentally ill citizens. The deinstitutionalization movement has shown us what happens when we try to deal with a social problem of enormous magnitude with an unintegrated, piecemeal approach. We've learned what a mess we can make of things when we don't know exactly what we're trying to accomplish-or why. And the effects of building a complex system on a foundation of mistaken beliefs has never been more apparent.
Flawed assumptions and their far-ranging effects
We can attribute most of our problems with providing decent living environments for the mentally ill to some basic assumptions that we made at the very beginning of the deinstitutionalization movement. Perhaps most important and pervasive was the almost insurmountable human tendency to believe that other peoples' minds- even those of people with severe mental illnesses- work in a manner similar to our own.
Schizophrenia and the other major mental illnesses were long believed to be "functional disorders" as opposed to the "organic" mental disorders. Psychiatrists thought that there was really nothing wrong with the brains of these people- they just weren't working properly because of problems with stress or imbalanced brain chemicals.
As a result we assumed that once the hallmark hallucinations, delusions, mania, and other severe symptoms of the disorders were controlled with medications the individual should be pretty much "normal"- like us. The programs and strategies that we devised to care for mentally ill people were generally ones that made sense to us and would work for us.
We assumed that once we released people from institutions they would promptly and willingly show up at the newly established " Community Mental Health Centers" to receive their care, just like anyone else who needed ongoing medical treatment and went to their outpatient clinics.
Of course we thought that these people would take their medications regularly. The fact that even optimal treatment would still leave many disabling symptoms unrelieved hadn't yet become obvious. The idea that many patients wouldn't be able to tell that they were ill was never considered.
Our assumption that they would return to "normal" living situations upon leaving institutional care was unquestioned at first. Clients that weren't able to make the transition to community living were quickly tucked away in crowded nursing homes and half-way houses that were little different than the asylums that they replaced. We've been in a reactive mode ever since, always scrambling to find places for mentally ill people to live but never having any semblance of a master plan or a way to develop and test the new assumptions that we've so sorely needed. The only thing that everyone has been able to agree on is that anything in the community must be better than those nasty asylums.
The belief that our clients would work in mainstream jobs once their medications were adjusted has carried through to the present day too. Even the most ardent advocates of Evidence Based Practices are still able to conveniently ignore the "evidence" that shows how useful supportive employment can be for clients trying to establish a meaningful life in the community. Everyone wants these people to work but little is done to give them a fighting chance at employment. It's difficult to get past the idea that they could work in competitive jobs if only they'd try just a bit harder.
Any enlightened system of mental health care will have to be consistent with the many things that we've learned about the human brain in these past fifty years. Until we can examine and replace the flawed assumptions that we've built upon it's going to be impossible to truly construct something better.
Is what we have now really so bad?
While statistics can be used in all sorts of nefarious ways, there are still a lot of people who just won't believe any argument that isn't backed by numbers. So a review of a few pertinent health care statistics is in order.

Mental illnesses account for over fifteen percent of the burden of disease in established market economies, such as the United States. This is more than the disease burden caused by all cancers combined.
At least one in five American adults is affected by mental illness in any given year. Some recent estimates suggest that this number may actually be much higher.
Health care costs have risen year after year, and now account for 15.5 percent of the U.S. gross domestic product. Health care spending was projected to top $1.9 trillion in 2005, about twice what is spent on education or defense.
Advocates for single-payer systems believe that about half that cost goes to waste, unnecessary services, bureaucracy, and other unneeded expenses.
More than 44.3 million Americans have no health insurance, and tens of millions more are underinsured. Private corporations pay less than 20% of health costs.
Nearly a third of the 1.6 trillion dollars spent on health care in America goes to duplicative care or treatment that fails to improve patient health. While Americans pay more for health care than other developed countries, we receive fewer services. We rank twelfth among thirteen industrialized countries in sixteen basic health indicators.
Dr. Steffie Woolhandler of Harvard Medical School points out that "we are already spending enough to provide every American with superb medical care - $5,775 per person this year [2003]. That's 42% higher than in Switzerland, which has the world's second most expensive health care system, and 83% higher than in Canada."
Typical government estimates put the figure for billing fraud and abuse at 10 percent of annual spending, amounting to over $150 billion annually.
The pharmaceutical industry receives about 18 % of each health care dollar. Since 1997 the industry has spent over 450 million dollars on lobbying, campaign contributions, political advertising, and public relations. It retains over 650 lobbyists in Washington D.C. and over 1,000 more at the state level.
Prescription drug spending grew at an average rate of 12.4% per year from 1993 to 1998, compared with a five percent average growth rate for overall health expenditures. The pharmaceutical industry has been the most profitable industry in America for each of the past ten years. In 2001 it was 5 ½ times more profitable than the average of all other fortune 500 companies. Profit margin in 1999 was 18.6%.
In 2000 the profits of one drug company- Merck- were 6.8 billion dollars larger than the combined profits of the Fortune 500 companies in the airline and entertainment industries.
Drug companies will argue that that sort of profit is necessary to support the research and development of new drugs. But tax credits - public subsidies - pay for 50% of all drug company research. So the poor taxpayer pays on both ends. We support research into extremely expensive and overpriced new drugs, then we pay outrageous profits to the drug companies so that we can supply these drugs to our poorest and most disadvantaged citizens.
When a recent study tried to compare new antidepressants it found that the research is almost too biased to really make comparisons. 96% of the medication trials were sponsored by or had at least 1 author affiliated with a pharmaceutical company. The remaining trials did not report funding sources.
A team of Boston University researchers says $950 billion each year- roughly half of America's annual health care expenses- are just wasted. The money goes to unnecessary administrative costs, profit, artificially inflated drug prices and fraud. One of the researchers points out that if only a third of the waste was cut from medical expenses the nation would still save more than $300 billion a year.
A December, 2002 report for the state of Massachusetts, designed to develop a statewide plan for "universal health care with consolidated financing," reported that 40 percent of every health care dollar spent in that state goes to administrative costs.
Other estimates vary but it looks like at least 30% of each health care dollar goes to administration, or the processing of paperwork. In America we spend almost as much on professionals who never see a patient -but instead attempt to make those who do treat patients more accountable- as we do on care providers. Anyone familiar with our mental health system, with its vague and shifting criteria for both diagnoses and service eligibility, will tell you that administrative costs are likely to be much higher than in the more "medical" specialties.
Here in Minnesota, at a time of unprecedented demand for psychiatric services, the number of licensed mental health beds decreased by over 15% from just 1996 to 2001.
Some commentators have stated that the rush to get consumers out of mental hospitals and into Medicaid-eligible programs has contributed to 200,000 mentally ill persons becoming homeless and nearly 300,000 being incarcerated in jails and prisons across the country.
From 1999 to 2001 emergency room psychiatric visits increased by almost 40% in Minnesota. Emergency room mental health visits for 15 to 20 year olds increased by 68% during the same period.
In 1999 an estimated 18% of American schoolchildren children met criteria for having an "emotional and behavioral disorder" which would qualify them for some assistance. Five percent were "severely disturbed". Yet only 2% of kids received EBD services and those were concluded to be largely ineffective.
Two thirds of juvenile detention centers end up locking up mentally ill youths because there is no place for them to receive appropriate treatment. 71 centers in 33 states said they were holding mentally ill youngsters who had not been charged with a crime.
The three largest psychiatric facilities in the U.S. are Los Angeles County jail, Rikers Island jail in New York City, and Cook County jail in Chicago.
Albert Einstein once said "Not everything that can be counted counts and not everything that counts can be counted". That's certainly the case when it comes to health care numbers. Should we ignore problems in our mental health system if costs were to somehow drop below the 70 billion dollars per year that we currently spend? If we could get the number of mentally ill people living with homelessness, poverty, or squalor down to just a hundred thousand would we say that's good enough and neglect those people?
Would it be OK if only a quarter of each tax dollar devoted to mental health was wasted?
Numbers can be tweaked to say just about anything. Just look at what the drug companies do with them. But anyone who wants to take the position that America's system of health care in general - and our mental health system in particular - are in good shape will have an awful lot of powerful statistics to explain away. It's pretty clear that our mental health system is expensive and inefficient. The dollars we spend often end up in the wrong hands. The number of people that we're being asked to support is growing dramatically. If we continue on our present course the whole thing is going to collapse on itself.
And the numbers capture just a small part of the problem we're facing.
Scattered site apartments as the gold standard of community care?
When deinstitutionalization began most of the people suffering from severe mental illnesses gravitated to our large urban areas. Some ended up in single room occupancy hotels or rooming houses but many of those aging and shabby places were torn down when inner cities were rebuilt.
The next options were frequently nursing homes and crowded halfway houses. But it gradually became apparent that many of them offered no greater shot at recovery than the asylums that people had been forced to leave.
The effort then shifted to putting everyone into mainstream, individual, scattered site apartments. For a lot of clients managing an apartment on their own was just too much to ask. Paying rent, shopping, food preparation, and housecleaning all required energy, motivation, and organizational skills that many were lacking because of problems with their brains. Then there was the social aspect to consider. Most people without mental illnesses don't live alone in isolated apartments. We tend to live with other people.
The newest approach is to keep clients in the solo apartments but beef up the services that are brought to them. Now if more help is needed we've created an army of workers who will come to the person's apartment to try to help them get by. Case managers, Assertive Community Treatment teams, and dozens of contracted home health agencies now exist to provide in-home services.
We've created special waivers to pay for in-home services for the elderly, the brain injured, and people at risk for nursing home placement. Shopping, meal preparation, housecleaning, transportation to appointments, help locating work, day treatment, medication monitoring, and a host of other services are available. Whatever it takes to help the person to stay afloat in their apartment can now be obtained. The problem is that this level of in-home support is only available to a small percentage of clients and only when the Federal programs will pick up the tab for them.
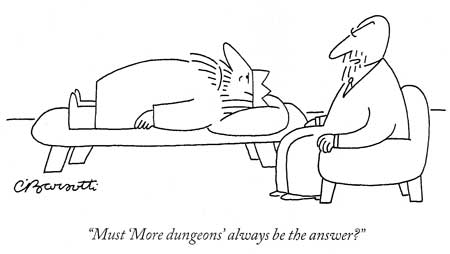
Of course the only way to qualify for this level of help is to demonstrate that you really need it. We insist that our clients be dysfunctional. Inability to care for oneself is a requirement to get services and it must be continuously demonstrated to remain eligible for them. Our clients know that if they show any glimmer of the ability to function more independently they can lose all of the help that the system provides in very short order.
This is still a more humane system than what has existed before. Sometimes it works tremendously well for individuals. But there are a great many people who don't benefit from this system. Their neuropsychological deficits that remain even after effective medication treatment are often too extensive to be addressed by bringing services into the home for a few hours per week.
Of course there is no guarantee that anyone will receive optimal medication treatment in our mental health system. And even if it's offered there is no assurance that clients will actually take these medications. Non-compliance rates with psychotropic medications among psychiatric outpatients populations typically run at over 50%. And many patients end up on such a long list of medications that it's hard to tell whether sedation, confusion, and problems with functioning are a part of the illnesses themselves or a result of our attempts to treat them.
Obviously, there are a lot of other problems with this system. The array of apartments available when a person is getting around 600 dollars per month in Social Security Disability Income or other entitlement programs is very limited. Surviving on that sort of sub-poverty income would be an enormous challenge to almost any of us. Going the next step to begin to recover a decent quality of life is, of course, another matter entirely.
Many of these clients have multiple evictions (we call them "unauthorized detainers" here) or other problems on their housing records that would immediately disqualify them for good apartments, even if they could find and afford them. Others don't have the skills to locate apartments, negotiate leases, or obtain furnishings. Yet our system is based on the idea that these people will get mainstream apartments from regular landlords. The fact that the landlords of decent apartments almost always have other prospective tenants to rent to - people that may be much more attractive as renters - is overlooked.
So much can go wrong
Given the current housing crunch, our clientele's general unattractiveness as tenants, and their poverty, it is natural that they'd end up in the worst buildings and neighborhoods. The high turnover rate in these apartments is also understandable. Even on the occasions when decent housing is somehow arranged a lot of things can go wrong.
Many clients are vulnerable to exploitation and quickly have their apartments taken over by drug dealers, other indigent people, or even family members, and lose their apartments as a result. Others fall behind in their rent when forced to choose between giving their limited dollars to landlords or meeting other basic necessities. And still others simply choose to live on the streets because they have no way of stretching their disability income far enough to cover both housing and food.
Studies find that over half of our severely mentally ill people abuse alcohol or street drugs (and curious double standards are often applied by helping professionals). But why wouldn't they use those things to try to feel better? What other sources of pleasure do they have in their lives? What do they have to lose?
Most non-mentally ill people don't quit using drugs or alcohol until they are facing some sort of negative consequences as a result of their use. Losing a job, relationships with loved ones, or their self-respect are common motivators for people to become sober. But many of our patients don't even have these things to lose in the first place.
Drug and alcohol abuse and their associated behaviors often result in problems leading to eviction as well. Many clients have been given the false impression that if they decide to drink, or use marijuana or other drugs, they should stop their psychiatric medicines. So they end up dealing with the effects of substance abuse and the abrupt stoppage of their medications at the same time. The clinical triad of psychotic decompensation, medication non-compliance, and substance abuse is one of the most common causes of hospitalization- and the loss of one's housing- in our mental health system.
The day-to-day lives of mentally ill people living in these situations are often quite grim and empty. Many are afraid to leave their homes, especially after dark. The few apartments that are available to our impoverished clients are often run down and clustered in undesirable, high crime neighborhoods. There may be no opportunities for pleasure or socialization. Transportation can be inadequate or unavailable. The idea of obtaining good employment may be just a fantasy. None of us would choose this sort of life for our own children.
Social isolation is an enormous problem for many of these people. Even bringing someone into the apartments for several hours per week leaves the person alone for the vast majority of their time. These are people who often have tremendous difficulties with human relationships. They may not initiate or maintain contact with others easily. They can be overwhelmed by closeness when it does occur. Clients are often shunned or stigmatized in their own neighborhoods.
The hours that our patients are the most isolated, lonely, and anxious are typically during evenings and early mornings - times when no mental health professionals are available and going out of their apartments is the riskiest. Recent studies have found that people who are lonely frequently don't sleep well. Lack of sleep only compounds their preexisting problems with brain functioning. A cycle of increased depression and anxiety or destabilization of psychotic or manic conditions, which in turn lead to further impairment of sleep, often results.
One of the strangest ironies in our mental health system is that the people who have the most problems with being alone - people who may even feel like a ghost or spirit or demon is always in the room with them or those who just have no prayer of stumbling into a satisfying social relationship - are the very people that we've decided should live all by themselves for the rest of their lives in scary apartments.
In reality, there are many people for whom living in scattered-site apartments simply does not work. Problems with planning, foresight, judgment, impulse control, and substance abuse are just too tenacious. Bringing in thousands of dollars in supportive services each month does nothing to really change the situation. Yet many clients will often insist that they want an apartment and refuse to look at other alternatives simply because the other available options are so limited, and so distasteful to them.
Are we spending our tax dollars wisely?
The emphasis on holding individual, mainstream apartments as the goal for everyone carries a wide variety of associated problems. A major one is that this system is extremely expensive. In fact the average patient receiving these community supports through Medical Assistance funded programs in Minnesota gets over $3000 per month in services. Some people's care runs as high as $12,000 -15,000 per month. That's just to cover the workers coming in to the home and some basic supports. Food, rent, transportation, and psychiatric care are additional. And the medication costs for these individuals can easily contribute another one to two thousand dollars per month.
Just think about the implications of this system of care. We see lots of clients each and every day who absorb 60,000 dollars per year in goods and services without being able to return anything to society. Many patients cost the system far more than that. Any experienced clinician can think of all sorts of customers who have incurred treatment costs in excess of a million dollars during their careers in the mental health system.
The average worker in our country now makes about 45,000 dollars per year and pays roughly $10,000/ year in taxes. So if every single dollar that an average worker went to support one of these mentally ill adults ( without spending anything on roads, schools, politicians, bombs, or other social programs ) that would mean that six of those average workers have to work all year to support that one very common client.
As expensive as these in-home supports can be, the money isn't the only issue. After all, we spend a great deal more on average to provide community living for a mentally retarded citizens than we do for each mentally ill person, despite the growing evidence that the problems experienced by both groups are just as "real" and rooted in structural brain changes. The "Developmentally Disabled" have more powerful advocates and the average layperson or politician doesn't have to deal with underlying assumptions that mentally retarded people "just aren't trying hard enough". So the "D.D" clients get a much richer funding stream, more supports, and better places to live.
The real inequity comes when we look at how our resources are distributed among the mentally ill people themselves. Our society has taken a relatively small group of clients, provided them with these very expensive supports, and essentially pretended that this is what our safety net for mentally ill people looks like. This approach is a lot like trying to build a pyramid from the top down. It has left countless mentally ill people homeless or living in environments that provide them with no meaningful chance for recovery whatsoever.
A major contributor to this approach is that competition between local and Federal agencies to see who will ultimately provide for these clients. A State or County system may be perfectly OK with providing thousands of dollars per month in supports as long as it's the Federal government that's picking up the tab but when dollars have to come out of their own budgets there is suddenly nothing left at all for the mentally ill. And at this very moment those Federal administrators are looking for some way out of this. They know that there's a very long line of people who are trying to get these supportive apartments and budgets are already stretched thin.
The sad fact is that we spend enough on our present mental health system, with its multifaceted bureaucracies and mega profits for drug company stockholders, to ensure a decent living environment for everybody. But only a small percentage of clients get the help that they deserve. And most taxpayers don't care which branch of government is paying the bills when the money is ultimately coming out of their own pocket anyway.
More inefficiencies
In our goofy system even going grocery shopping can easily end up costing much more for the staff's time than for the actual food. Sometimes it's necessary to send two staff members out for even routine business with clients - either because of the client's own potential for misbehavior, problems with other people living in the buildings, or the dangerous neighborhoods that the apartments are located in.
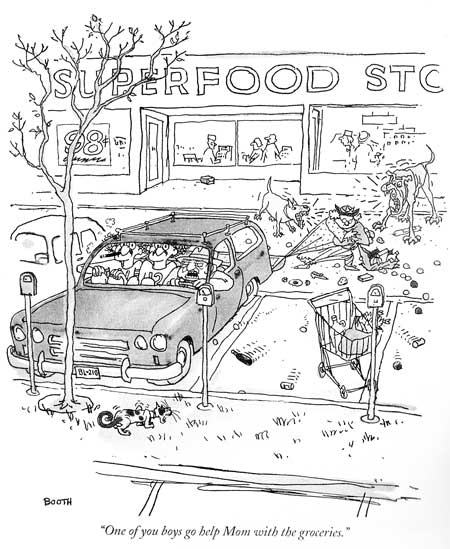
Many times when support staff arrive at the apartment the client is not there and the visit has to be rescheduled. Fear of strangers, beliefs that they don't really have mental illnesses or need help, and difficulties maintaining schedules are just a few of the reasons why so many times services are set up for our clients but have to be abandoned after only a month or two.
Compounding matters is the fact that the agencies that provide workers to come to people's apartments to help out are chronically short-staffed. Our system of community mental health care is now shifting towards a "privatization model" but the employees of these for-profit companies are frequently underpaid and lack even basic training about mental illness. And those profit seeking companies have no incentive to go out and find the patients who are too sick to come into the clinic for their infrequent appointments.
The companies that contract to provide workers to support the patient in their apartments are in competition for staff with fast food restaurants and other generic, low paying jobs. Many workers flee as soon as they see what working with the mentally ill is really like so there is an enormous amount of turnover in personnel. Waiting lists to get a new "service provider" assigned are often lengthy. This instability is particularly difficult for our clients as they generally tolerate change poorly and have difficulty establishing trusting relationships under the best of circumstances.
For the many clients who can't manage to live "independently", the options are often worse. Until recently, the backbone of our housing system for the severely mentally ill in Minnesota have been what we called "Rule 36 Facilities". These halfway houses for mentally ill people were charged with the task of preparing the client for independent living in the scattered site apartments. That goal was often impossibly difficult to meet. Those facilities were only designed to keep people for nine months or so before having them ready for apartments and many clients never made much progress at all towards acquiring the independent living skills that the system wanted for them.
Recent changes have now limited the time a person can stay at these places to 90 days - again with the assumption that something magical will take place which will make living alone in low-end apartments a satisfying lifestyle. We also seem to expect that a few months in these "Intensive Residential Treatment" facilities will somehow correct brain problems that may be hard-wired into their nervous system. Of course it's very expensive to put clients into these places. Very few of the patients living in the facilities manage to fall below that $60,000 / year mark.
Our halfway houses- by whatever name- are often poorly staffed and little actual therapy or preparation for independent living may take place. The neuropsychological deficits that people have as a result of their mental illnesses are not the kind that can easily be remedied and even if learning takes place in one environment there is no guarantee at all that it will transfer to a new one. Plus, the clients are typically crowded into rooms with one to three other clients. We'll see that this can have enormous effects on their nervous systems.
For many clients, those halfway houses- though beset with problems- are still the places that do the best in terms of providing the amount of staffing, supervision, and social contact that the person needs to get by outside of hospital settings. But the clients have to move on in one way or another. This whole system now depends on people leaving in very short order.
While some people actually do move on to successful apartment living, our halfway houses have to rely on the fact that a great many clients will leave via hospitalization or eviction. The circuit from apartment to hospital to halfway house is a well-traveled one, with frequent stops at nursing homes and homeless shelters thrown in.
Other housing options are also beset with problems. Board and Care or Board and Lodge facilities almost always have multiple people per room. Therapies or meaningful activities are rarely provided. These places are very limited in the sorts of behaviors that they're equipped to deal with so once again evictions and dismissals via hospitalization are very common. And even putting patients up in those places doesn't give society much bang for its buck. Monthly rates just for the room and board are typically in the $1500 range and all of those other treatment and support costs don't go away.
Our mental health system is long on transitional living facilities but short on places to transition to. Despite all of our talk about providing people with places to live outside of hospital settings and delivering gads of expensive privatized services there is one word that is very rarely heard in our planning meetings these days. "Home" is just never mentioned. But who among us could ever establish a meaningful and satisfying life without one?
Couldn't we think of a more degrading term than "Adult Foster Care"?
The latest attempt to deal with our glaring lack of supportive housing for severely mentally ill people has been an emphasis on "Corporate Adult Foster Care". In some situations this has been an upgrade. Clients are typically housed in more homey environments and round-the-clock supervision is usually available. But problems have been quick to surface. A recent visit to one of these facilities proved informative.
A nice suburban rambler had been converted to an "Adult Foster Care" home for four mentally ill people. Two of the clients were doing something outside of the home when we arrived. The other two were sitting on a couch watching television like any other Americans. In the next room three professionals sat around a table. They looked a bit embarrassed and made a point of shuffling papers around as it was clear that there presence wasn't adding much.
The way to get the very expensive, round the clock staffing covered in a place like that involves having prospective patients screened by a team of nurses -using forty page screening forms developed by distant bureaucrats. The nurses review the clients care needs and determine how much Medical Assistance money should be devoted to the support for each individual. Their reports eventually come before yet another team of administrators who then reviews the findings and make the formal allotments of dollars. Once again we spend huge amounts of money in an effort to determine whether a given client should receive services, and to what extent.
Of course the needs of any particular client can change significantly over time. They may look terrible on paper one month and be in a much better mental spot the next. But if the system actually works and the individual does get better things can quickly unravel. The need for expensive, hands-on staff goes down as people stabilize.
When the next six month review is done these clients fall into a different spot on the reimbursement formula. The dollars devoted to their care decrease. So the Foster Care homes can lose the money that they need to provide staff if their clients really do develop a more satisfying and independent way of living. The facilities then have to either cut back on the workers that they employ, find new clients with higher care needs, or cook the books to make it look like their existing clients need more help than they really do.
A recent study found that two out of five Doctors "fib" for their patients in order to avoid insurance denials. When pillars of the community like us are twisting the truth in order to get people's care funded it's pretty certain that there must be a lot more "fibbing" in other parts of the system. "Rounding upward" to make clients look more sick and needy is a constant at all levels of our mental health system. It's an unfortunate game but one that everybody is required to play.
When there is much bureaucracy and disincentive to improvement involved in a system the one thing that can be counted on is wastefulness. All sorts of strategies get played out as facilities jockey to have their clients get the highest care need ratings possible. Everyone familiar with this system has examples of people who aren't really very impaired getting up to twenty four hours of "Personal Care Attendant" time per day while other very ill people get nothing at all.
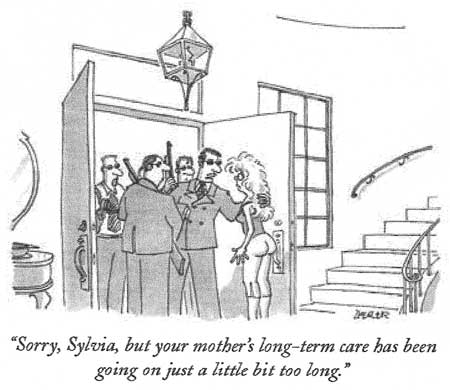
Dollars may be readily doled out as long as the stream coming in from the Federal government is robust but sooner or later the Feds catch on. They try to make the money harder to access by adding increasing layers of paperwork and new regulatory requirements. More staff are necessary to fulfill the needs for charting, "treatment planning", and proving that "measurable goals" have been achieved.
As attempts are made to shift the care of mentally ill people to supported apartments staffed with Medical Assistance-funded personnel the Feds respond by cutting both the dollars available for apartments and for the support staff. The jobs of all the administrators necessary to play this expensive game are, of course, quite secure. But none of this truly benefits the mentally ill people that are seeking help with basic problems of living.
We devote so much of our mental health budgets to things that have nothing at all to do with food, shelter, medicine, or decent employment options that the patients themselves sometimes seem like just an unfortunate nuisance.
When do psychiatric hospitals become a pricey residential safety net?
Once people are hospitalized on psychiatric wards- whether because of increased symptoms of their illnesses or because it was the only way to get out of a bad living situation- there is an immediate emphasis on returning the person to the community as quickly as possible. Hospital beds are a very scarce and expensive resource. Costs of a thousand dollars per day or more are very common. Yet chronic mentally ill people often do or say whatever is necessary to get into the hospital because it may be the only way that they know to get help finding alternative housing.
The number of hospitalizations that are ultimately prompted by the need for an apartment or a wish to move to a different one would be stunning to the uninitiated.
It's also extremely common for our clients to use hospitals when they're broke. Some savvy clients even count on a couple of hospitalizations per year as a way to get extra income. When they're discharged they may have a month or two of disability checks that they didn't have to spend because everything was taken care of on the psych ward. It may be the only time in a given year when they feel like they have enough money to get by.
It's not unusual for clients to seek hospitalization as a way to address medical problems that they couldn't otherwise negotiate. Admission to a psychiatric ward ensures access to physical exams, consultations, medications, and outpatient appointments that would be very hard to acquire in other ways. A lot of our people don't have a relationship with a primary care doctor. Getting admitted to psychiatry can be much more comfortable than the long waits in emergency rooms that so many people now depend upon for outpatient medical care. Many of us can even recall patients who managed to be admitted to psychiatric wards to get help with dental problems.
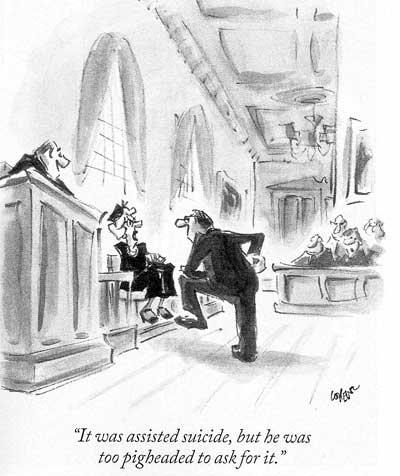
Our mentally ill citizens are frequently put into a position that they either must become very ill or emphasize suicidal intent in order to get into the hospital. Few emergency room Doctors will refuse admission to people that are saying that they're going to die if they aren't admitted. This situation has become so commonplace that insurance companies will now question whether a hospitalization was "medically necessary" if there isn't sufficient documentation to show that admission was a matter of life or death.
When the mentally ill in Minneapolis are deemed ill or dangerous enough to warrant hospital treatment they're sometimes hospitalized in distant communities or even other states because of a bed shortage in the metropolitan area. Severely ill patients are often denied hospital admission because beds are filled with people who have, by necessity, emphasized their dangerousness to self or others.
More and more often we're seeing that mentally ill people who really need hospitalization are in competition for hospital beds with people who don't even have severe mental illnesses. Chemically dependent people are having a real tough time in our society and many have learned that the mental health system is a good place to go for support. Many of them seek hospitalization as a way to get connected with entitlements and, especially, apartments. And they have already learned those magic words that are necessary to be granted admission.
Many clients bounce from hospital to group home to apartment, living in several different places each year. Again, these are people who by virtue of problems with their nervous systems are the least capable of handling the stresses inherent in these kinds of changes.
And then there are always some mentally ill clients who some simply feel and function better with the level of human contact, care, and supervision that hospitals provide. Some of us see people who routinely ask whether it will ever be possible for them to live in the old State Hospitals again. Of course the things that they miss have nothing to do with "treatment". For some, those hospitals were the closest thing they had to a home in their adult lives.
That other safety net

More mentally ill people sleep in shelters and prisons each night than sleep in hospitals. This is a picture of one of the homeless shelters in Minneapolis. You need a special voucher to stay here so it costs our system twenty dollars per night to keep someone in these wall to wall bunk beds. Obviously, that 600 dollars per month could finance an apartment but that's just not the way things work. It's hard for most of us to appreciate the impact on a person's mental health that comes from living in such crowded and demoralizing conditions.
When drug trials are carefully studied one things that becomes very obvious is the truly amazing strength of the placebo effect. Inducing hopefulness and the expectation of improvement are still clearly the most powerful weapons in our psychiatric armamentarium. But we forget that this effect works in both directions. When people are faced with hopelessness, demoralization, and the absence of any chance to better their situation the resulting negative effects on their mental functioning can be just as powerful. Our current mental health system has all sorts of deleterious effects on the mental health of the very people that it's supposed to be helping.
One of the strangest things about our current system of community care for the mentally ill is that there is no way to predict who will end up in an apartment with several thousand dollars per month in services brought in, and who will end up in a shelter or on the streets. How ill you are really isn't a determining factor- in fact being severely mentally ill may actually decrease the likelihood that one of those apartments with expensive supports will materialize.

In Minneapolis "Secure Waiting" is where you end up if you have no place else to go and weren't fortunate enough to have won a lottery mat at one of the church shelters or obtained a voucher to sleep in the crowded bunk beds. About 250 people per night sleep on mats placed on the floor, only two or three inches from the next person's mat. A crowded, chaotic place to sleep and standing in lines at soup kitchens is the true safety net that our society provides for its mentally ill people. And even this is costly. The tab for running Secure Waiting runs around 1.5 million dollars per year.
Not surprisingly, many mentally ill people opt out of this bizarre system altogether. People who work in the shelters report that it's often the very sickest people that end up sleeping in the streets. One of the most frequently cited reasons that our homeless mentally ill give for living on the streets or under bridges is that they just doesn't feel safe being around so many other people in the shelters, with all of their associated problems of poverty, theft, assaults, and substance abuse.
The bottom line is that our current system of providing supportive housing for our chronic mentally ill people isn't working well for the clients themselves or for our society. This system is very cumbersome, inefficient, and extremely expensive but does not provide a meaningful and humane safety net that can be counted on to support our most incapacitated citizens.
A return to the asylums?

The need for a sufficiently secure and stable environment doesn't go away when we reach adulthood. For mentally ill adults the living environment is crucially important. When you think about it, until a little over 50 years ago the only thing that we really had to offer people with severe mental illnesses was a specialized environment. We used to call them asylums.
Asylum is regarded as a dirty word these days but it wasn't always that way. It originally meant a sanctuary, a refuge, an inviolable place that you couldn't be taken from against your will.
The meaning of the word shifted over the centuries, in response to what so many facilities for mentally ill people actually became. Many of these places were overcrowded, poorly staffed dead ends that isolated patients from the rest of society. The people living in them were sometimes treated cruelly or subjected in inhumane psychiatric treatments. Anybody arguing for a return to the asylums of the past would quickly find himself strung up by the advocates for mentally ill people, with good reason. But we shouldn't ignore some basic facts about those old approaches to mental health care.
In the better State Hospitals of old patients felt relatively safe and secure. The hospital grounds and buildings were often beautiful and calming. There were opportunities for socialization. Friendships and marriages were possible. Families knew that their loved ones would be fed, sheltered, and cared for. Most importantly, there was little chance that people would be shuffled from place to place against their will. Many patients stayed in these hospitals for decades, came to regard them as their home, and strenuously resisted the forced return to the community that they were eventually faced with.

Old State Hospital: At least the sleeping mats had legs

In the old state hospitals when people were crammed together they had real beds to sleep on. More staff were available. Patients often worked at various types of jobs. And they didn't have to worry about where they'd be sleeping at night.
Given the current emphasis on expensive new psychotropic drugs, it may seem unthinkable that any person with a severe mental illness could have ever lived without them. But antipsychotic and antidepressant medications didn't show up until the 1950's and patients somehow managed to survive in the asylums before then. We lose sight of the fact that when the environments were good enough some people even went on to recover from severe mental disorders.
In our current system of community care more than one in four nursing home residents is institutionalized with a primary mental health diagnosis. About thirty percent of our nations jails routinely hold mentally ill people that are not charged with a crime- just because there's no other place to put them. Many mentally ill youngsters are warehoused in juvenile detention facilities due to a lack of community programs suitable to meet their needs. Shelters are turning mentally ill people away every night.
So any effort to frame the closing of the old State Hospitals as completely positive should be looked at with skepticism. There were clearly some things that they did a better job of providing than the system we're saddled with now. Anyone arguing that the motivations for dismantling the State Hospital system are purely "client centered" should be met with similar skepticism. The decisions about the integrity of our safety net are being made by people who are primarily concerned with financial factors and political power.
Anyone who takes the position that things have been routinely better for these people since the movement from asylums to community treatment is on rather shaky ground. In truth, we've done a lousy job of replacing our asylums. We didn't know much about mental illness when we started the process and we haven't been able to overcome bureaucratic inertia enough to allow a change of course. If we don't find a new direction we're headed for disaster.
A new set of basic assumptions is sorely needed
As we begin to build a sane system of mental health care we certainly don't want to use the same set of assumptions that we built the current mess on. The "medical model" idea that brain problems would be corrected once and for all with medications sure hasn't held up. Neither have beliefs that clients would comfortably return to normal community apartments, clinics, and jobs once they left the large institutions. We'll need a little sturdier foundation this time around.
An entire set of principles to build a new system on will be offered up for attack in an ensuing chapter. For now let's consider just a few basic assumptions that might serve us better than those old ones:
Providing enriched living environments specifically tailored to meet the needs of people with severe mental illness will be both clinically useful and cost effective.
Using a comprehensive, integrated approach to providing those environments will make more sense than doing it piecemeal again.
Developing teams of service professionals that work together will be more efficient and effective than recreating the scattered, disorganized system that we currently have.
It makes more sense to develop and test clinical models of supportive housing, then figure out exactly what sorts of administrative help is needed than to keep doing it in reverse order. One ongoing characteristic of mental health bureaucracies is their tendency to keep reorganizing themselves- at tremendous cost- but those reshufflings rarely translate into any palpable improvement in care for the consumer.
If we do this right we'll be able to create a system that provides everyone with a decent standard of living and an opportunity to make their life better through their own efforts - for less than the cost of the leaky safety net that we provide now.
An examination of the brain problems that mentally ill people must deal with, and the things that they need to function at their best, is the most logical place to begin our look into the future of mental health care.